
Lymphoedema after breast surgery was something that was talked about before and after the removal of my lymph nodes. I had been fine with no symptoms until towards the end of 2019. I noticed after exercising a few tiny lumps on my at-risk arm. on my at-risk arm.
I booked an appointment to see my breast surgeon Dr Ash Kothari (head Onco-Plastic Breast Surgeon and Clinical Lead) and a referral was made for the Lymphoedema Clinic. There was so much I needed to know about lymphoedema and its effects on the body. My body.
I was able to talk on camera with one of Guy’s Lymphoedema specialists Practitioner.
What is Lymphoedema?
Lymphoedema is a long-term (chronic) condition that causes swelling in the body’s tissues. It can affect any part of the body but usually develops in the arms or legs. Lymphoedema happens when the lymphatic system is not working properly.
Lymph fluid normally flows through a network of lymph vessels. These lymph vessels connect to a group of lymph nodes. The nodes act as a filter. They trap or destroy anything harmful that the body does not need.
Inside the lymph nodes are white blood cells, also called lymphocytes. These white blood cells attack and break down bacteria, viruses, damaged cells or cancer cells.
You have nodes throughout your body. Lymph nodes vary in size. Some are as small as a pinhead, and others are about the size of a baked bean.
The number of lymph nodes in the body differs from person to person.
The lymph fluid carries the waste products and destroyed bacteria back into the bloodstream.
Symptoms of Lymphoedema:
The main symptom of lymphoedema is swelling in all or part of a limb or another part of the body. It can be difficult to fit into clothes, and jewellery and watches can feel tight.
At first, the swelling may come and go. It may get worse during the day and go down overnight. Without treatment, it will usually become more severe and persistent.
Other symptoms in an affected body part can include:
- an aching, heavy feeling
- difficulty with movement
- repeated skin infections
- hard, tight skin
- folds developing in the skin
- wart-like growths developing on the skin
- fluid leaking through the skin
There are 2 types of lymphoedema – primary and secondary lymphoedema which have different causes.
Primary Lymphoedema:
Primary lymphoedema is caused by alterations (mutations) in genes responsible for the development of the lymphatic system. The faulty genes cause the parts of the lymphatic system responsible for draining fluid to not develop properly or not work as they should. Primary lymphoedema often runs in families, although not every child born to someone with the condition will develop it themselves.
Secondary Lymphoedema:
Secondary lymphoedema develops in people who previously had a normal lymphatic system that then becomes damaged. (As in my case) It can have a number of different causes. Some of the most common causes are explained below.
Surgery for Cancer:
Treatment for cancer can involve surgery to remove sections of the lymphatic system. The surgeon will try to limit damage to your lymphatic system, although this is not always possible. There’s a particular risk of lymphoedema occurring after treatment for any cancer where lymph glands are removed.
Some of the more common cancers where this happens are:
- Breast Cancer (As in my situation)
- Skin Cancer (melanoma)
- Gynaecological Cancers – such as cervical cancer and vulval cancer.
- Genitourinary Cancers – such as prostate cancer or penile cancer.
Radiotherapy:
Radiotherapy uses controlled doses of high energy (radiation) to destroy cancerous tissue, but it can also damage healthy tissue. If radiotherapy is needed to destroy cancerous cells in your lymphatic system, there’s a risk that the lymphatic system could become permanently damaged and unable to drain fluid properly.
Infections:
An infection, such as cellulitis can sometimes cause lymphoedema. Severe cellulitis can damage the tissue around the lymphatic system, causing it to become scarred. Filariasis can also cause lymphoedema. Lymphatic filariasis is a parasitic disease caused by microscopic, thread-like worms. The adult worms only live in the human lymphatic system and block lymph drainage. It’s a common cause of lymphoedema worldwide.
Secondary Lymphoedema:
Secondary lymphoedema develops in people who previously had a normal lymphatic system that then becomes damaged (that’s me again). It can have a number of different causes. Some of the most common causes are explained below.
Inflammation:
Medical conditions that cause tissue to become red and swollen can also permanently damage the lymphatic system.
Conditions that can cause lymphoedema:
- Rheumatoid Arthritis.
- Eczema.
Venous diseases:
Diseases that affect the flow of blood through the veins can cause lymphoedema in some people. The abnormal or damaged veins can cause fluid to overflow from the veins into the tissue spaces. This overwhelms and eventually exhausts the parts of the lymphatic system responsible for draining this fluid.
Some venous diseases that can lead to lymphoedema include:
- DVT (deep vein thrombosis) – a blood clot in 1 of the deep veins in the body
- Swollen and enlarged veins (varicose veins) – where poor drainage of blood in the veins causes higher vein pressure and more fluid overflowing into the surrounding tissues
Obesity:
Obesity is another possible cause of secondary lymphoedema. People who are obese, particularly those who are severely obese, have an increased risk of developing swollen body parts. It’s not clear exactly why this is, but it’s been suggested that the extra fatty tissue affects the lymphatic channels in some way, reducing the flow of fluid through them. In these cases, weight loss is an important part of treatment and even just starting to lose weight can make a big difference to the swelling.
Trauma and Injury:
In a small number of cases, lymphoedema can be caused by an accidental injury to the lymphatic system. For example, it can sometimes occur after a road traffic accident where there’s extensive bruising or soft tissue loss.
Immobility:
Movement and exercise help lymph drainage because muscle activity surrounding the lymphatic vessels massages fluid into and along them. Reduced movement can therefore lead to lymphoedema because the fluid in the lymphatic system does not get moved along. For example, people who have limited mobility for a long period of time as a result of an illness, nerve damage or arthritis may be at risk of lymphoedema.
Diagnosing Lymphoedema:
There are specialist lymphoedema treatment centres where individual symptoms can be investigated and treated.
Measuring Limb Volume:
In some cases, tests to calculate the volume of an affected limb may be carried out.
These may include:
- using a tape measure – to measure the circumference of the limb at certain intervals to calculate its volume
- water displacement – where the affected limb is placed in a tank of water and the amount of water that’s displaced is measured to calculate the volume of the limb
- perometry – where infrared light is used to measure the outline of an affected limb and calculate its volume
Bioimpedance Testing:
During a bioimpedance test, small metallic discs called electrodes are placed on different parts of your body. The electrodes release a small, painless electric charge that’s measured using a handheld device. Changes in the strength of the current can indicate the presence of fluid in your tissue.
Imaging Tests:
Imaging tests may also be used to help diagnose and monitor lymphoedema.
These Include:
- A lymphoscintigram – where you’re injected with a radioactive dye that can be tracked by a scanner; this shows how the dye moves through your lymphatic system and can check for any blockages
- An MRI scan – a strong magnetic field and radio waves are used to produce detailed images of the inside of your body
- An ultrasound scan – high-frequency sound waves are used to create an image of the inside of your body
- A CT scan -X rays and a computer create detailed images of the lymph nodes.
Lymphoedema Treatment:
The recommended treatment for lymphoedema is decongestive lymphatic therapy (DLT). DLT is not a cure for lymphoedema, but it can help control the symptoms. Although it takes time and effort, the treatment can be used to bring lymphoedema under control.
The above treatment (DLT) is the method that is being used to treat my secondary Lymphoedema.
Massage:
To begin with, you may receive specialised massages called manual lymphatic drainage (MLD) – usually carried out by a specialist therapist – to move fluid from the swollen areas into working lymph nodes, where it can be drained. Your lymphoedema therapist will also teach you a range of simpler massage techniques that you or your carer can use during the maintenance phase of treatment to help keep the swelling down. These self-massage techniques are known as simple lymphatic drainage (SLD).
Decongestive Lymphatic Therapy (DLT):
There are 4 components to DLT:
- compression bandages – to complement exercise by moving fluid out of the affected limb and minimise further build-up
- skin care – to keep the skin in good condition and reduce the chances of infection
- exercises – to use muscles in the affected limb to improve lymph drainage
- specialised massage techniques – known as manual lymphatic drainage (MLD); this stimulates the flow of fluid in the lymphatic system and reduces swelling
DLT is an intensive phase of therapy, during which you may receive daily treatment for several weeks to help reduce the volume of the affected body part. This is followed by a second phase called the maintenance phase. You’ll be encouraged to take over your care using simple self-massage techniques, wearing compression garments, and continuing to exercise.
This treatment phase aims to maintain the reduced size of the affected body part. You’ll have reviews every few months to check how your treatment is progressing.
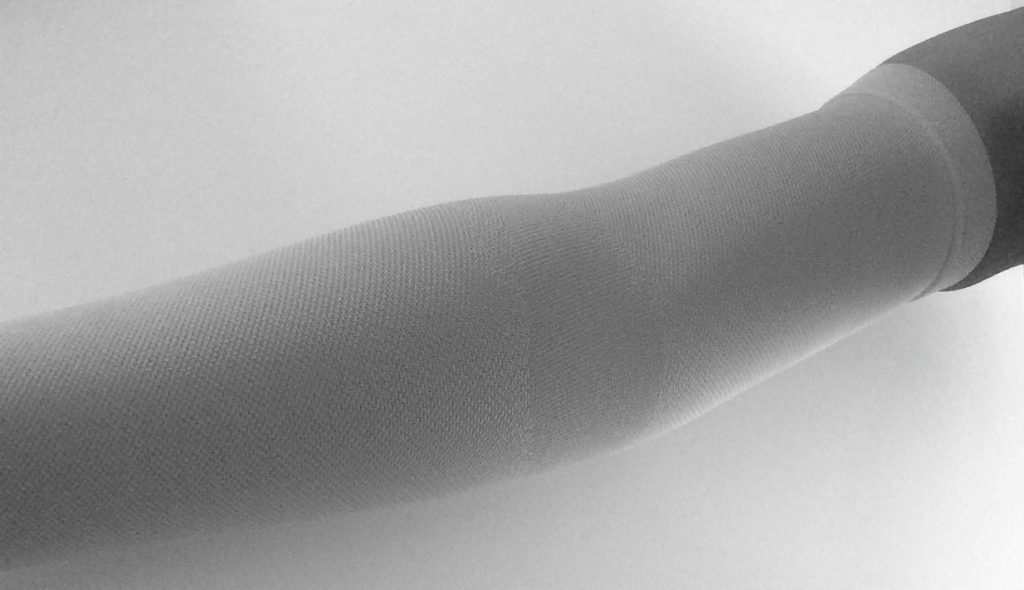
Compression Bandages and Garments:
Below are the compression bandages that I wear every day on my right arm for a few hours while exercising and afterwards. It really helps with the lymphatic build up on my at-risk arm.
The compression bands work in the most incredible ways, after only an hour of wearing one, the fluid build-up literally vanishes.

Unlike blood circulation, the lymphatic system has no central pump, such as the heart to move to the fluid glands. Instead, it uses the massaging effect of surrounding muscles to move the fluid. This is why exercise is important.
Compression bandages or garments, such as sleeves, gloves, stockings or tights, fitted over affected limbs act as a counterforce to muscles. This stimulates more effective lymph drainage. The combination of exercise and compression encourages the fluid to move out of the affected limb. (I follow this method every day)
Compression garments may also be applied after a massage session to prevent fluid from accumulating in the limb again. Velcro wraps may be used instead of bandages or compression garments. These are easier to apply yourself. You’ll be taught how to correctly apply compression garments or Velcro wraps so you can continue using them during the maintenance period.
Skin Care:
It’s important to take good care of your skin to reduce your risk of developing an infection, such as cellulitis.
Movement and Exercises:
Your lymphoedema care team will help devise an exercise and movement plan designed to strengthen and stimulate the muscles involved in lymph drainage.
They’ll also help you lose weight if you’re overweight. Your exercise plan will be tailored to your requirements and ability.
Your plan may involve specific limb exercises, as well as gentle activities that involve the whole body, such as swimming, cycling and walking.
Massage:
To begin with, you may receive specialised massages called manual lymphatic drainage (MLD) – usually carried out by a specialist therapist – to move fluid from the swollen areas into working lymph nodes, where it can be drained.
Your lymphoedema therapist will also teach you a range of simpler massage techniques that you or your carer can use during the maintenance phase of treatment to help keep the swelling down. These self-massage techniques are known as simple lymphatic drainage (SLD).
Surgery:
In a small number of cases, surgery may be used to treat lymphoedema. There are three main types of surgery that may be useful for the condition:
- Removal of sections of excess skin and underlying tissue (debulking)
- Removal of fat from the affected limb (liposuction)
- Restoration of the flow of fluid around the affected section of the lymphatic system – for example, by connecting the lymphatic system to nearby blood vessels (lymphaticovenular anastomosis)
These treatments may help reduce the size of areas of the body affected by lymphoedema.
Liposuction:
The accumulation of fat is a significant feature of lymphoedema swelling. Liposuction is where a thin tube is inserted through small cuts (incisions) in the skin to suck fat out of the tissue.
It can be used to remove excess fat from an affected limb to help reduce its size. After surgery, you’ll have to wear a compression garment on the affected limb day and night for at least a year to help keep the swelling down. While it’s not possible to completely prevent lymphoedema, the following advice may help reduce your chances of developing it.
Skin Care:
The part of your body affected by lymphoedema is more vulnerable to infection of the build-up of fluid within the tissues.
Any cuts in your skin can allow bacteria to enter your body and may quickly develop into an infection. Skin infections can also damage your lymphatic system and cause lymphoedema to develop.
You can reduce your chances of developing skin infections by:
- Not having injections or blood pressure readings in the affected area whenever possible.
- Treating cuts and scratches immediately with an antiseptic cream.
- Using insect repellents to prevent insect bites.
- moisturising the skin daily to keep it supple – a GP can prescribe a suitable cream.
- Avoiding very hot baths and showers – the heat from saunas, steam rooms and sun beds may increase the swelling.
- Using sunscreen with a high sun protection factor (SPF) to prevent sunburn.
- wearing gloves for gardening and household tasks to avoid cuts if your upper limbs are affected.
- Using anti-fungal powder to prevent fungal infections in your skin or feet if your lower limbs are affected.
- Cutting your nails with nail clippers.
- Seeing a chiropodist for foot and nail care – make sure you tell them you have lymphoedema.
- Wearing shoes that fit correctly and provide support on the top of your feet if your lower limbs are affected.
- Using an electric razor if you need to shave to reduce the risk of cutting yourself.
- Not wearing tight fitting clothes or jewellery.
Contact your doctor as soon as possible if you develop symptoms of a possible skin infection. These symptoms may include redness or a feeling of heat in the skin.
Healthy lifestyle:
Adopting a healthy lifestyle may help reduce your risk of developing lymphoedema and may also help control the condition if you already have it.
This includes:
- Eating a balanced healthy diet.
- Maintaining a healthy weight.
- Exercising regularly.
- Living an overall active life where you are not sitting or sleeping for long periods of time instead of being active.

Comments are closed.