A Port-a-Cath is a small medical device that is installed beneath the skin.
6. Port-a-Cath My Saving Grace
- 1. My Most Recent Scare
- 2. Chemo Prep The Second Time
- 3. Chemotherapy The Second Time Begins…
- 4. Chemo Side Effect The Second Time
- 5. What I’m Currently Eating
- 6. Port-a-Cath My Saving Grace
- 7. My Lockdown Support Team
- 8. ENT Surgery & Prep
- 9. Chemotherapy The Third Time Begins…
- 10. Chemo Side-Effects & Changes, The Third Time.
- 11. Journey Towards A New Recovery
On Thursday 8th October 2020, I was fitted with a port-a-cath at the Interventional Radiology Department at St. Thomas’ Hospital.
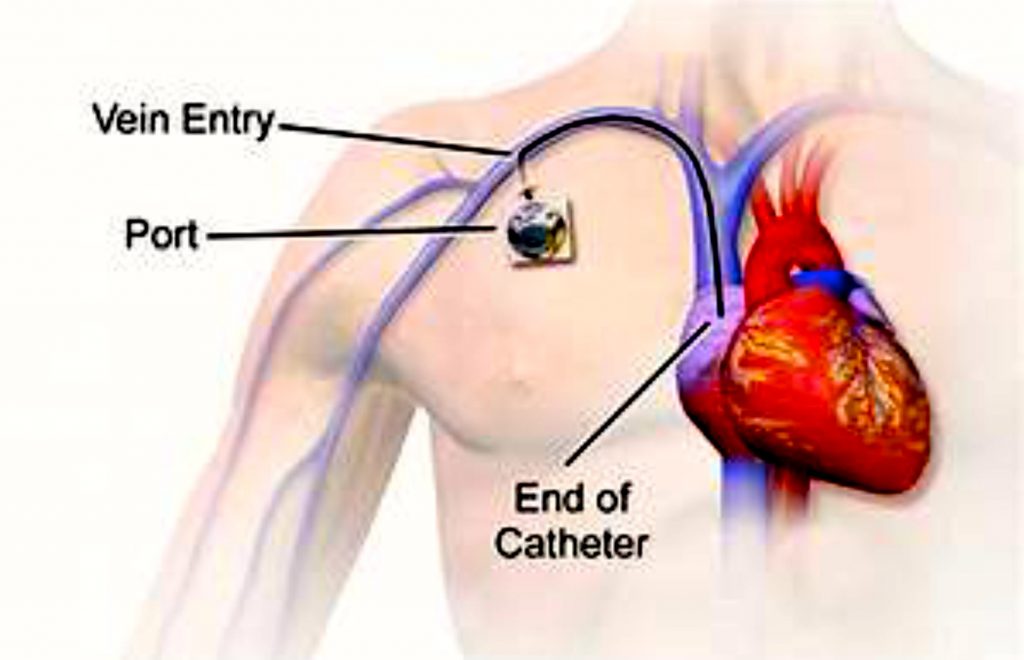
A port-a-cath is a small medical device that is installed beneath the skin. A soft, thin hollow plastic tube is known as a catheter. The tube is tunnelled under the skin with the tip sitting just outside the heart. A port or disc is inserted into the chest and attached to the tube.
These small, flexible tubes are placed in large veins for people who require frequent access to the bloodstream during treatment such as myself. This is a saving grace for me as the port can be left in for a long period of time.
The Brilliant Minds That Created The Port-a-Cath or Catheter: The first document indwelling CVC was created by Stanley E Dudrick in 1967. The first marketed CVC was made by James Broviac in 1973 and was a single lumen type intended for parenteral support. In 1979, Robert O Hickman created a larger version of the single lumen catheter with its intended use for bone marrow transplant patients.
In 1980 Robert R Uldall created the first hemodialysis catheter which was later refined in 1987 by Sakharam D Mahurkar who held the patent for this for many years. In 2000, Stephen R Ash modified the hemodialysis catheter by splitting the two lumens apart.
Procedure For My Port-a-Cath: I arrived at the Interventional Radiology department early, was assigned to a bed, given a gown, a pair of socks, and some blankets.
Then came the part I have been dreading, which is the blood work. Before my procedure can be done, my white blood cell (which helps fight infection) count needs to be rechecked because the previous test indicated my white blood count was slightly low.
The nurse assigned to me saw how small my veins were, so decided to call a doctor to try so that I’m not pricked too many times in order to get a workable vein. Dr Tom Gordon was a total delight and on the fourth attempt we got blood and he fixed a cannula for my procedure.
I walked into the theatre and it was freezing cold. There was a huge revolving ex-ray machine, screens, and monitoring devices. Lots of drawers and stools. I was instructed to lay on the procedure table then cover-up. I think there were four people in the room, two doctors and two nurses. They all introduced themselves but no one’s name stock apart from Dr Tom Gordon. I was covered up and the area prepped for the insertion.
Shortly after the introductions, there was a lot of talking amongst the doctors and nurses, lots of movements, and surgical pieces of equipment being brought out of the draws and placed next to the doctors. The area was made numb and the process began. Every now and then the nurses and doctors would ask how I was doing?
I would say about forty-five minutes later all was done and I was told it had gone well. I knew Dr. Gordon had done a good job on the procedure because I listened very attentively as he and his attending doctor worked. The senior doctor was impressed with the technique Dr. Gordon used and she told him so several times.
I heard the nurses checking all the tools used were still accounted for. The protective clothes were taken off me and I was wheeled back into the recovery room.

Back in recovery and under observation after the port-a-cath procedure at the Interventional Radiology Department at St.Thomas.’ I was offered something to eat and drink then monitored for two hours with continual vitals monitoring. Dr. Gordon came back for a quick chat then discharged me. I was given some plasters to change the dressing with instructions. My close friend Jane had already arrived so I was discharged to her.
Reasons The Port-a-Cath is My Saving Grace: I was first diagnosed with breast cancer (DCIS) almost five years. Since that diagnosis, I have had many tests done. A lot of those tests were in the form of blood tests which meant a needle was inserted into a vein on either my right, or left arm, in order for blood to be taken. By the time I started chemo the first time around, I was having several blood tests a week.
My first major surgery then was a mastectomy and reconstruction combined with the removal of all the lymph nodes underneath my right arm and from the walls of my right chest. This meant that from that moment onwards only my left arm could be used for all my blood tests as the removal of the nodes leaves the right arm vulnerable to infection and lymphoedema.
Chemotherapy the first time around was administered on the large vein on my left arm and by the time chemo was finished that vein had become hard, dark and unresponsive.
Once all was done and I was given the all-clear, I still had regular blood tests done which went from every month to every six weeks then to every three months, and finally to every six months. With those tests, I suffered greatly because of my tiny collapsing veins.
The veins on my left arm were exhausted from the constant needle puncture which started almost five years ago so during my first consultation with Dr. Kristeleit I mentioned my concerns about my exhausted veins and how I didn’t think they could cope with all that was to come and he happily suggested to have a port inserted. That was the first time I’d heard of a port-a-cath. He said the team would call me with an appointment and tell me all about it.
Since the port-a-cath insertion on my chest, the anxiety of going in for my weekly blood test has greatly reduced. There is a process to accessing the port and the port nurses do a great job with me every single time and always get a good flow of blood.
I remember thinking to myself after the first time my port-a-cath was accessed, why wasn’t I offered this little gem the first time around? Life would have been so much easier because there were always at least three to four attempts to find a vein before success.
During a discussion with Dr Gordon who inserted the port before it was done, he had mentioned that it worked brilliantly on children and the elderly too. During my research, I discovered that originally the port was created to aid mothers with babies with eating difficulties.
I can honestly say that this device has made my treatment so much more bearable by taking away my anxiety about the repeated needle punctures I had been enduring for years. The inventors should be proud.
My Port-a-Cath was removed on Thursday 14th April 2022 at St. Thomas’ Hospital in the Interventional Radiology Department. It has been a part of me for almost two years.


- 1. My Most Recent Scare
- 2. Chemo Prep The Second Time
- 3. Chemotherapy The Second Time Begins…
- 4. Chemo Side Effect The Second Time
- 5. What I’m Currently Eating
- 6. Port-a-Cath My Saving Grace
- 7. My Lockdown Support Team
- 8. ENT Surgery & Prep
- 9. Chemotherapy The Third Time Begins…
- 10. Chemo Side-Effects & Changes, The Third Time.
- 11. Journey Towards A New Recovery
