...an 8-hour session, and then 5 hours of observation...
3. Chemotherapy The Second Time Begins…
- 1. My Most Recent Scare
- 2. Chemo Prep The Second Time
- 3. Chemotherapy The Second Time Begins…
- 4. Chemo Side Effect The Second Time
- 5. What I’m Currently Eating
- 6. Port-a-Cath My Saving Grace
- 7. My Lockdown Support Team
- 8. ENT Surgery & Prep
- 9. Chemotherapy The Third Time Begins…
- 10. Chemo Side-Effects & Changes, The Third Time.
- 11. Journey Towards A New Recovery
Today is Monday 2nd November 2020: I received an email containing instructions, videos, and information regarding my entire chemotherapy treatment. This had to be watched and questions are written down before my chemo video call prep with one of the nurses happening much later on the same day. The session was to inform me of what would happen during chemo, places to turn to for help, and tips on what to do to maintain any symptoms that may develop.
Today is Wednesday 4th November: Chemotherapy for the second time begins today. I arrived at Guy’s Hospital Cancer Village by 7 AM. Prep start time was 7.30 AM.
I was welcomed very warmly and because I was very early got to choose where I would like to sit. I chose the nearest section to the window as the winter sun was out and strong. Shortly after that, the prep began with lots of information on how the morning would go. My first treatment has been split into two days and today is the shorter day. Tomorrow will be an eight hours session with five hours of observation in there too.
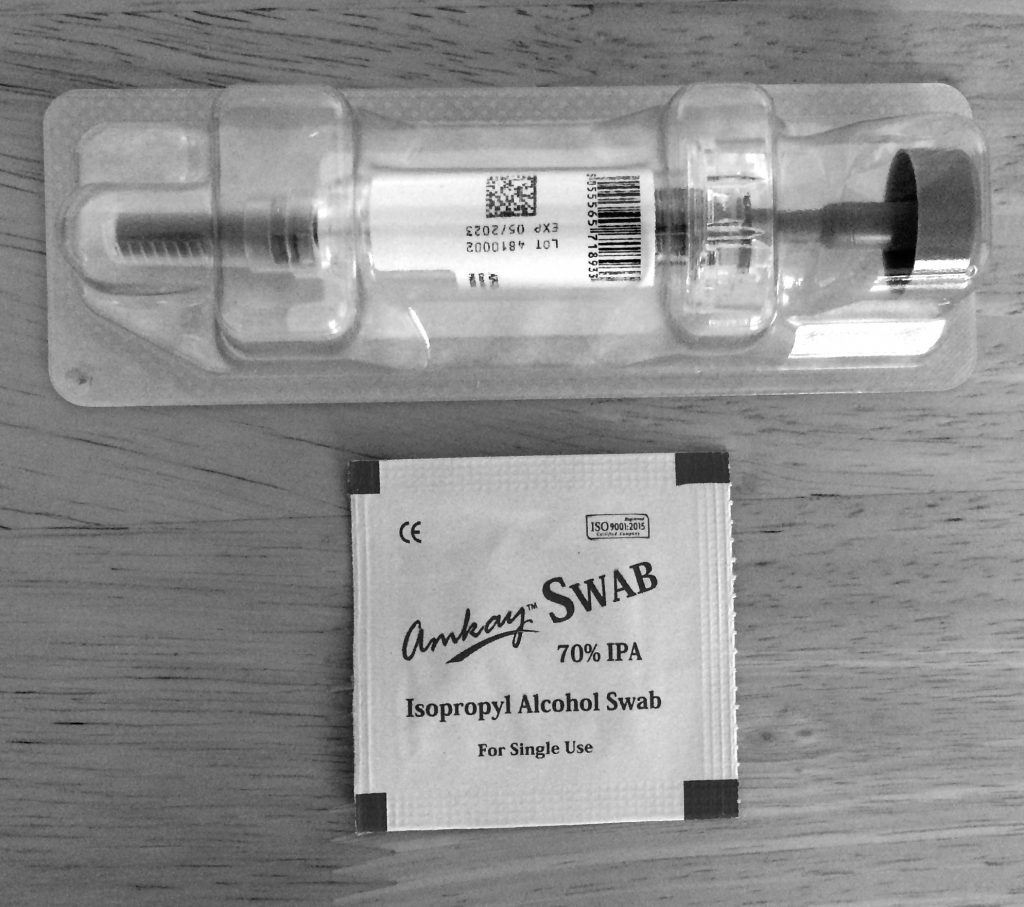
I was taken into a room to have a cannula inserted into my port-a-cath. It was flushed and ready for my first second round of chemo.
My chemo this time around is a combination of three drugs. One will be administered today and two tomorrow.
Started with saline followed by the first of the chemo drugs called Trastuzumab, a targeted therapy used to treat breast cancer and is usually given with chemotherapy.
This works by targeting specific proteins (receptors). Trastuzumab and Pertuzumab (which will be my combined two) both work by targeting specific proteins (receptors). They are the best combination for the type of cancer I have.
This took about an hour followed by another saline infusion which lasted about thirty minutes. Was observed throughout then was free to go home with lots of reading materials about my treatment and what was to be expected.

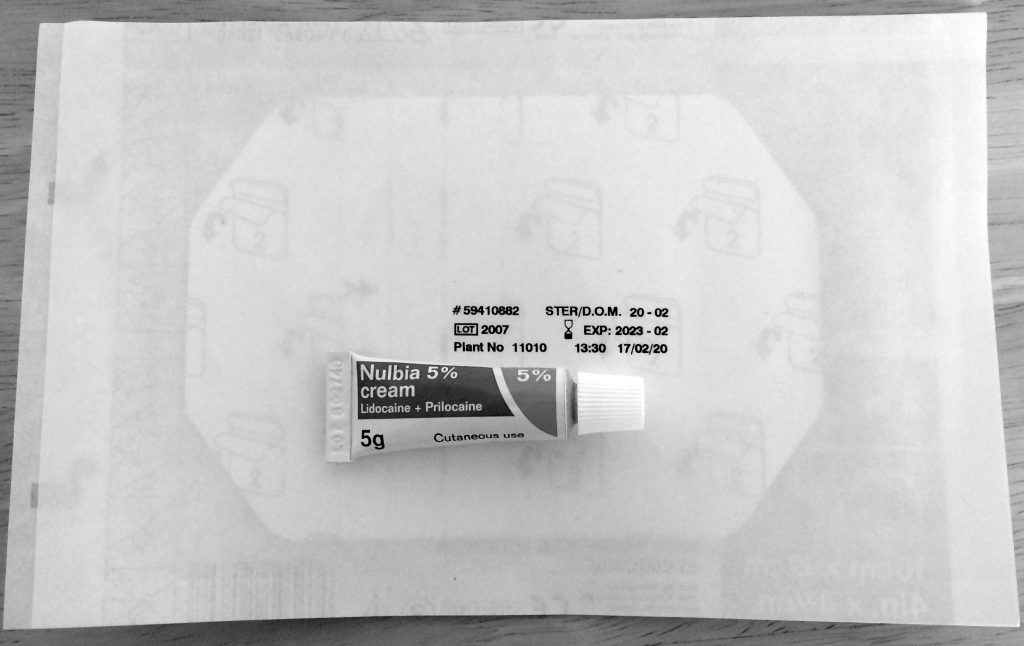
Today is Thursday 5th November: Day two of my first round of chemo for the second time. Again I arrived very early for my session so I used the opportunity to put on some numbing cream on the access area of my port-a-cath then covered it with plaster as instructed. This will take effect in about thirty minutes. The cannula inserted into the port is done via a needle, the numbing cream will help numb the pain of the needle insertion.
Again I opted for a chair by the windows although it was very foggy outside. The first point of call was to get the cannula into the port-a-cath. The numbing cream really helped to
Started with an anti-sickness tablet, some antihistamine to stop any allergic reactions, some steroids then a saline flush followed by a drug called Paclitaxel, used to treat ovarian, breast, and non-small cell lung cancer. Paclitaxel can be given on its own or in a combination with other chemotherapy drugs.
Another saline then Pertuzumab, a targeted therapy used to treat breast cancer and usually given with chemotherapy. This works by targeting specific proteins (receptors). Trastuzumab and Pertuzumab both work by targeting specific proteins (receptors). They are the best combination for the type of cancer I have.
This was followed by another saline flush then the five hours of observation started with regular checks by my brilliant chemo nurse named Nurse Jing. Thankfully there were no adverse reactions to any of the chemo meds I was administered today so after about four and a half hours I was cleared to leave so I called a very dear friend who picked me up and dropped me off at home.
From Next week there will only be one visit a week for Paclitaxel chemotherapy and at the end of every month, I will have all three chemo drugs together then the cycle starts again in December till my cycle is completed. I’m back at the chemo lounge on Wednesday the 11th of November for a lovely dose of Paclitaxel chemotherapy.
Today is Wednesday 11th November: Arrived early, as usual, used some numbing cream on my port entry, covered it with a plaster then proceeded to the chemo lounge. The port was accessed as normal then a blood test was carried out to ensure my body was ready for another hit.
The full blood count indicated that my platelets were slightly low. My body needed a little more time to recover back to a safe platelet level. I’m to return next Wednesday to continue with my treatment.
Platelets: A low platelet count, also known as thrombocytopenia is a common chemo side effect. When you get a cut or bruise, platelets form plugs in the blood vessels to stop the bleeding. Chemo destroys cells that grow rapidly, including those in the bone marrow that produce platelets.
Today is Wednesday 18th November: My Paclitaxel “hit” day at Guy’s Cancer Lounge. Today I decided to use the numbing cream on the port access area from home. At the chemo lounge, the port was accessed for a full blood count, and for the first time, I didn’t feel the needle going into the port. From now on I’ll be applying the numbing cream just before I leave home.
Blood work came back and while my platelet level was back to normal, my neutrophils count was slightly low and because of this, it is not advised to give me a chemo infusion. If I was to fall ill with such a low count, I would be very ill indeed.
Neutrophils: Are a type of white blood cell that is central to our immune system. As part of our innate immune defense, neutrophils act as the first-line responders to infection, attacking bacteria, viruses, and other pathogens.
I was told to wait another week for my levels to get better, sent home. The Onco team treating me would be informed for directions. I had previously been scheduled to see Dr Kristeleit, my oncologist, for a follow up so the timing couldn’t be better. I started writing down questions to put to him on Monday 23rd November.
I am now two weeks behind with my chemo treatment plan so hoping for answers and resolutions next week as I would like this process to be concluded within the time frame I had been given.
Today is Monday 23rd November: The appointment with my Onco consultant Dr. Kristeleit was this morning. I didn’t see him personally but a lovely lady from his team. We discussed my treatment not going as planned because of my low neutrophil count.
A plan had been made to investigate. Haematology, a branch of medicine that focuses on blood, has requested I needed to have a bone marrow biopsy so they can take a closer look at my blood for analysis. On further discussions, I was informed that the fact that my body had already gone through both chemotherapy and radiotherapy before could be a factor but they needed to be sure.
We discussed the side effects I’m currently having and I was given a prescription for the acid indigestion I get after every meal and a mouthwash to try.
While Haematology does its thing, I will carry on with my treatment of the Trastuzumab and Pertuzumab without the Paclitaxel for now.
I received a call from the Haematology Team early Monday evening to get the process started with an explanation of the process. 🙁

Today is Wednesday 25th November: My appointment at Guy’s Cancer Lounge for the antibodies Pertuzumab and Trastuzumab without Paclitaxel went really well. The port-a-cath was accessed and a cannula was inserted. A flush first followed by thirty minutes of Pertuzumab and saline then an hour of Trastuzumab and more saline. The port was flushed again and I was free to leave.
Today would have been the beginning of cycle two had my neutrophils not been too low which interrupted the completion of Paclitaxel during cycle one. The tests next week by the haematology team should hopefully shed some light on my neutrophils count.
Today is Wednesday 2nd December 2020: I had a Bone Marrow Aspiration and Trephine Biopsy at Guy’s Hospital in the morning.
A Bone Marrow Biopsy is the removal of marrow from inside the bone. Bone marrow is the soft tissue inside bones that helps form blood cells.
An Aspiration removes a small amount of marrow in liquid form for examination.
The samples were taken from my right pelvic bone. I assumed the foetal position laying on my left side. The skin was cleaned with antiseptic and some local anaesthetic was injected into a small area of skin and tissues over the bone. A little sting then became numb. I was also offered some breathing gas which made me quite lightheaded and a little more relaxed.
To Aspirate bone marrow fluid, a needle was pushed through the skin into the bone and a syringe was used to draw out some liquid bone. Sadly the bone cannot be numbed so I felt the extraction but it was only for a few seconds.
To Biopsy the Bone Marrow, a thicker, hollow needle was inserted into the bone. It was then rotated around as it’s pushed slightly forward to force a small sample of bone marrow into the middle of the needle. Again as the bone cannot be numbed I felt every drill but it was only for about five (5) seconds.
All the needles were removed and the site was dressed. I was observed for twenty minutes laying in bed. The insertion area was checked and redressed and I was free to go home. The results will be with my consultants in just over a week.
Walking was a little uncomfortable and once the local anaesthetic wore off the pain was managed with painkillers.

The dressing will be changed again in two days and by the end of the week, the entry point should close up. The inner healing would take a while and I have been advised against running for about a month though I can start walking the running route two weeks from now.
Today is Monday 14th December: My appointment with the Onco Breast team today was with the lovely Dr. Andrea Podvez. She is one of the doctors under my consultant Dr. Hartmut Kristeleit’s team.
We talked about how I had been feeling since our last meeting and after the bone marrow biopsy. I filled her in and she informed me the biopsy results are still pending, however, the haematology team will discuss in detail their findings at my appointment with them next week.
She measured the lymph node by my right collar bone and confirmed it had shrunk slightly.
She checked my neutrophils count during chemo almost four years ago and she explained the levels were very similar and in some cases the same counts. She informed me that if haematology confirmed all was good from their end then she is happy I can resume Paclitaxel as part of my chemotherapy treatment.
I left her then went to the chemo nurses to access my port for another blood test in preparation for the next antibodies on Wednesday morning.
Today is Wednesday 16th December: Today is the third session of the antibodies without Paclitaxel at the chemo lounge at Guy’s Hospital. I arrived early as usual. My chemo nurse introduced herself and after the usual pleasantries, it was time to access the port and get me ready for the treatment.
A flush first followed by thirty minutes of Pertuzumab and saline then an hour of Trastuzumab and more saline. The port was flushed again and I was free to leave.
This is the last session of my treatment till early January 2021 which is about two and a half weeks away. I will get the bone marrow biopsy results next week.
Today is Monday 21st December: My appointment with Clinical Haematology Dr. Richard Dillon at Guy’s Hospital was earlier this morning. I had a bone marrow biopsy to ensure that all was well under the microscope. This was requested because of some instabilities with some of my blood count.
The consultant assured me that all was fine after looking under the microscope. There were no abnormalities. Thank God!!
There was one more result pending (genetic mutation), this would be provided in the New Year. He also stated it was nothing to worry about though if anything was found, it would just mean monitoring via a blood test once a year.
Today is Monday 4th January 2021: My appointment with the Clinical Onco Breast team was this morning. I was seen by my consultant Dr Kristeleit. After the New Year pleasantries, he asked how I had been feeling? I walked him through and we talked about the good results of the bone marrow biopsy.
Dr Kristeliet confirmed I would be having the full cocktail of antibodies with Paclitaxel on Wednesday this week and pending my blood work resume the weekly Paclitaxel. I was then sent for my blood test in preparation for Wednesday’s chemo infusion.
I was met by the same lovely chemo nurse Hassan who accessed my port and drew blood just before Christmas. It was a quick and painless process. Minutes later I was free to leave.
Today is Wednesday 6th January: I arrived early at Guy’s Cancer Lounge. It’s my first chemo of this year. My blood count is all back to normal so I will be receiving my fourth round of the antibodies combined with my second hit of Paclitaxel chemo. I had applied the numbing cream on the port entry before leaving home.
I was called in by my nurse for the day and asked to choose where I would like to be treated. As always I chose a seat next to the windows. It all begins with the accessing of the port on my chest with a cannula then flushed and prepared for the infusion.
The antibodies are administered separately. The first called Trastuzumab is a targeted therapy used to treat breast cancer and is usually given with chemotherapy.
The second is Pertuzumab. Both work by targeting specific proteins (receptors). They are the best combination for the type of cancer I have.
This took about an hour each then followed with another saline infusion which took about thirty minutes.
The third drug started with an anti-sickness tablet and an antihistamine for any allergic reactions, some steroids then a saline flush followed by Paclitaxel, used to treat ovarian, breast, and non-small cell lung cancer. It can be given on its own or in a combination with other chemotherapy drugs.
This took an hour then I was free to leave. I return for my weekly infusion of Paclitaxel next Wednesday pending good levels of blood count.
Today is Wednesday 13th January: I arrived early at Guy’s Cancer Lounge as always, first for a blood test then a session of Paclitaxel pending a good blood count.
Sadly my neutrophils (which helps the body fight infection) count is slightly low to receive another hit of Paclitaxel chemo. So my lovely chemo nurse encouraged me to go home, relax and hopefully return next week with a better blood count. My Port-a-cath was flushed and I was free to go home.
Today is Monday 18th January: My second appointment with a haematology consultant revealed again that all is fine with no genetic mutation detected.
As my neutrophils count is normally only low by a few counts, the hematology consultant recommended an injection which would help with my counts to my Onco consultant Dr. Kristeleit. This will ensure that there would be no more delays with Paclitaxel chemo.
This was a relief and I was happy to hear there was a plan to help complete the entire chemotherapy plan. I went for a blood test in preparation for Wednesday.
Late Monday evening I received a call from my Onco consultant Dr. Kristeleit. He informed me my blood counts were all fine and at the right level for chemo on Wednesday but he would be adding three Filgrastim (ACCOFIL) injections to start on Saturday for three days so that there would be no delay with my next hit of the antibodies and Paclitaxel next week.
Filgrastim (ACCOFIL) belongs to a group of proteins called cytokines and is very similar to a natural protein (granulocyte-colony stimulating factor [G-CSF]) produced by your own body. Filgrastim stimulates the bone marrow (the tissue where new blood cells are made) to produce more white blood cells that help fight infection.
Today is Wednesday 20th January: I arrived at Guy’s Chemo Lounge early feeling optimistic and assured that I will receive Paclitaxel chemo today which would be a step closer to finishing the course.
My chemo nurse introduced herself and accessed my port-a-cath in preparation for the infusion. Pre checks were done and I was ready for the infusion. Starting with an anti-sickness tab and some antihistamine, steroids then a saline flush followed by Paclitaxel for an hour then another thirty minutes of saline flush.
My port was flushed and the cannula removed. I was handed the injections to be stored in the fridge till used. I requested a district nurse for the injections as I wasn’t sure I would be able to inject myself.
Today is Saturday 23rd January: A District Nurse is to pop into my apartment today to help with administering the first Filgrastim injection. I woke up early, had a quick shower and breakfast, took out the instruction manual from the pack in the fridge, and read it through a few times.
About 12 PM I received a call from the District Nurse who said she would be with me within an hour so I decided which part of my body to be injected, applied some numbing cream then covered it with a large plaster.
Thirty minutes before the arrival of the District Nurse, I took out the first Filgrastim injection out of the fridge to reach room temperature which aides for a more comfortable injection, took out the sterile wipes and laid out everything needed on a small sterile table then waited anxiously.

The District Nurse called while at the entrance to my apartment and anxiously I buzzed her in. She appeared fully masked holding her pair of gloves with a little medical bag, introduced herself and I showed her my ready prepared table while putting on my own face covering.
She went into my bathroom, washed her hands, and requested tissue to pat dry her hands. I showed her the section of my body to be injected which was covered with numbing cream and a large plaster.
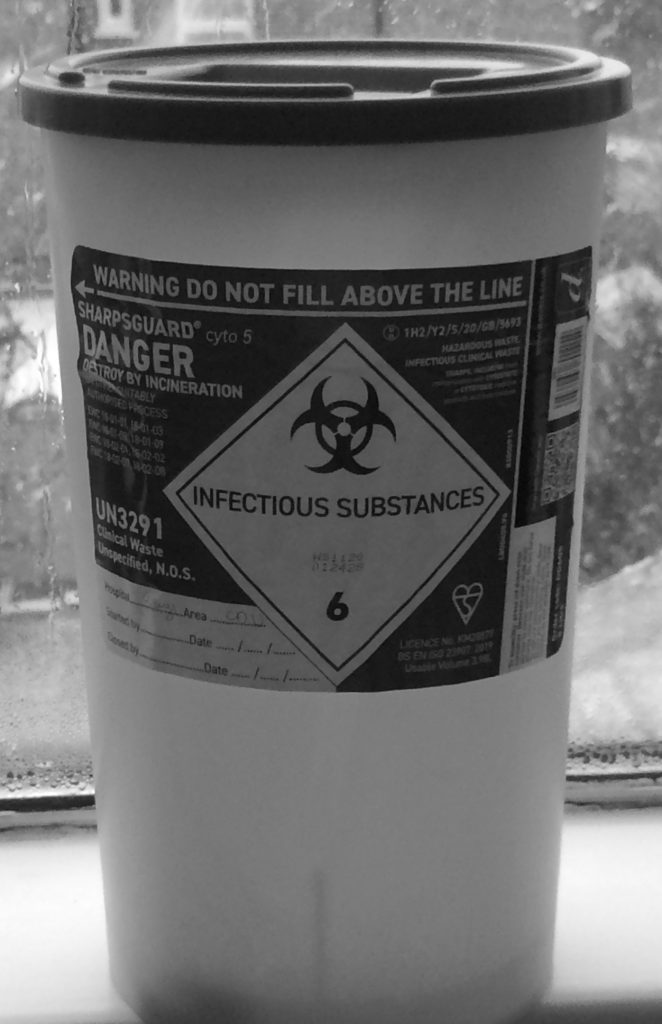
We talked briefly and she guided me through injecting myself. Although I was literally shaking the procedure went well and I felt no pain at all. She checked my stats and recorded them. We talked briefly while she sterilized her equipment and cleared the area used.
I was confident I could re-inject myself for the next two days to come and she was pleased that she would not be coming back into my sterile space. Actually, so was I.
Today is Sunday 24th January: The second Filgrastim injection will be administered at 1 PM this afternoon by myself.
The injections stimulate the bone marrow (the tissue where new blood cells are made) to produce more white blood cells that help fight infection e.g it will ensure my neutrophils count will be at the right level to receive chemotherapy on Wednesday.
I applied the numbing cream and plaster almost thirty minutes ago. The injection will be taken out of the fridge for thirty minutes before administering. In total the numbing cream would have been on an hour before I inject myself. My sterile table had everything that needed to be laid out and the timer was counting down.
The timer went off and nervously I washed my hands again, rolled up my top, took off the plaster, took off the lid of the injection and placed it back down, wiped the area with the sterile wipes, pinched some skin, at an angle inserted the full length of the thin needle into the side of my tummy, pushed down on the plunger till I heard the click indicating that Filgrastim has been fully injected then slowly pulled the thin needle out, released the plunger and the needle retracted. DONE!!! I could breathe again.

Today is Monday 25th January: Today’s Filgrastim injection will be administered slightly earlier today as I have an appointment to see my Onco consultant Dr. Kristeleit for a review and a blood test in preparation for Wednesday.
The numbing cream and plaster prep were done at 10 AM, thirty minutes later the injection was taken out of the fridge for thirty minutes before administering. My sterile table was laid out and the timer is counting down.
At exactly 11 AM, I repeated the process of administering mirroring exactly what I did on Sunday. The three syringes were placed in the bin below.

I got ready for my appointment at Guy’s hospital and just before I left home, applied the numbing cream on the entrance of my port in preparation for my blood test after seeing my Onco consultant.
Arrived at Guy’s Hospital early as always. The electronic notice board indicated my name should report to a room number so I acted as instructed. Knocked and went in.
I was greeted by the lovely Dr. Andrea Podvez who works on Dr. Kresteleit’s Onco team whom I’ve seen twice before. We discussed how I had been feeling and the side effects since we last saw each other just before the New Year. She talked about the Filgrastim injections and it’s short-term use just to ensure there were no more delays with my planned out chemo.
When all was done, She put out a request for a full blood check. I thanked her then left to await my call from the port blood nurses. I was called in and my port was accessed, flushed, blood drawn, flushed again and cannula removed. I was free to go.
Today is Wednesday 27th January: I arrived at Guy’s Chemo Lounge early for Cycle five of the antibodies and fourth Paclitaxel combined. It’s a long day as all three are administered one after another. The antibodies are thirty minutes each with a thirty minutes flush in between, followed by another thirty minutes flush then a one hour of the Paclitaxel followed by another minutes flush before my port is flushed and cannula removed.
Today is Saturday 30th January: The first of the three Filstagrim injections starts today and at the same time for the next three days.
Today is Sunday 31st January: Vaccination Day!! As the entire world is currently living with COVID-19 and its variations, everyone in the UK who chooses to has to be vaccinated starting with the elderly, their carers, doctors and nurses, and those considered as vulnerable such as me because I’m currently having chemotherapy.
After injecting the second Filstigrim injection I went off to my assigned GP Practise for the first of two vaccination jabs. After a rather long wait, it was finally my turn.
I was going to be vaccinated by a dentist who introduced himself, walked me through the vaccination process and how my arm and I may feel in the next few days. He gave me the jab which was painless, handed me a card with my details and what vaccination I was given then said I could go.
Today is Wednesday 3rd February 2021: Today I’m at Guy’s Cancer Lounge for my fifth Paclitaxel with a blood test first before the infusion begins.
My chemo nurse called me in, I chose a chair next to the windows as normal. The pre-checks were done and my port-a-cath was accessed, flushed and my blood rushed to the lab. About thirty minutes later, blood counts were confirmed as fine and the process began for a Paclitaxel infusion.
Starting with an anti-sickness tab and some antihistamine to stop any allergic reactions, steroids then a saline flush followed by Paclitaxel for an hour then another thirty minutes of saline flush.
My port was flushed and the cannula removed. I was given six Filgrastim injections last Wednesday and three injections have been used already with three more still stored in the fridge for this week. I start injecting from Friday 5th February.
Today is Friday 5th February: I started the morning by injecting myself with the first of the three Filgrastm injections.
The numbing cream and plaster prep were done earlier, thirty minutes later the injection was taken out of the fridge for thirty minutes before administering. My sterile table was laid out and thirty minutes later, following the injection instructions, I performed the task. Two more to go for this week.
My Appointment With ENT Consultant: I saw Mr. Alex Rovira this afternoon at Guy’s Hospital. We talked about my progress with chemotherapy and he looked at the lymph node on my collar bone.
Again he said if and when told to remove it by the oncology team he would be ready. He looked through my notes and said he would schedule our next appointment as a telephone consultation. I thanked him and left.
Today is Wednesday 10th February: As usual, I arrived at the Cancer Lounge at Guy’s hospital early for port blood first then for my sixth Paclitaxel chemotherapy.
My lovely chemo nurse called me in and I was asked to choose my chair for treatment. A place next to the windows like normal and the prep began.
The pre-checks were done and my port-a-cath was accessed, flushed and my blood sent off to the lab. Shortly after that my blood counts were confirmed as fine and the process began for a Paclitaxel infusion.
My port was flushed and the cannula removed. My nurse reminded me to ensure I start the Filstagrim injections from Friday 12th February. Got home feeling extremely tired so I slept till dinner time. This is highly unusual for me to sleep during the day but I went with it.
Today is Monday 15th February: Two things happened to me today. I was at Guy’s Hospital early this morning for port blood in preparation for Wednesday’s chemotherapy infusion. That went very well and my lovely nurse was a delight.
Then back home on time for a telephone consultation a few hours later with a doctor from the Haematology Team. I went through all that had happened within the last two weeks.
The stomach cramps, the loose stool incidents, nausea and throwing up, the blisters inside my nose and constant nose bleed, the feeling generally unwell, the having no urge to eat, and my constant twitching pair of eyes.
A few adjustments will be made to some of my pre-meds before treatment begins on Wednesday. And the new tablet was added to my existing ant-sickness medication. Hoping for the best and always very thankful, we said goodbye.
Today is Wednesday 17th February: My first appointment today at Guy’s Hospital was at the Cardio-Thoracic Centre. While my heart is fine, this current chemotherapy can affect some hearts so this appointment is to ensure that my heart isn’t being affected.
On arrival, my starts were taken and all was fine. I was finally called in by the Cardio-Thoracic consultant who will conduct the heart CT scans. These scans use a safe amount of radiation to create detailed images to view my heart and blood vessels.
She said my heart was doing just fine and the results would be sent to my onco consultant. Cleaned all the gel off my chest, thanked the consultant then ran off to the Chemo Lounge in the next building.
Chemo Lounge: I arrived at the chemo lounge with about thirty minutes to spare so I signed in and waited to be called. Today is a long day as I have cycle seven which means I have the antibodies and Paclitaxel one after the other.
My chemo nurse called me in and my stats were taken before accessing the port. My port-a-cath was accessed and a cannula was inserted. A flush first followed by thirty minutes of Pertuzumab and saline then an hour of Trastuzumab and more saline.
The third drug Paclitaxel takes an hour. It started with an anti-sickness tablet, some antihistamine, and some steroids (the quantity of the steroids has been adjusted so hopefully my body will handle the treatment better) then a saline flush for another thirty (30) minutes.
My port was re-flushed and the cannula removed. I was handed some more Filstagrim injections to start on Friday to Sunday. It was an extra-long day and I thanked my chemo nurses for their help and headed home.
I was anxiously optimistic that the next ten hours would go well and I would not get any violent, painful stomach cramps, uncontrollable loose stool incidents, nausea and throwing up, constant nose bleeds, and the worst of them all feeling generally unwell and extremely low after this infusion.
Today is Wednesday 24th February: The infusion for my eight Paclitaxel at the Guy’s Cancer Lounge was this morning. I arrived for a port blood test first to ensure my counts were at the right level for another hit.
My chemo nurse for the morning called me in and assigned me to a seat. My port was accessed, flushed and blood drawn. This was sent off to the lab urgently. My stats were done and all looked good. Shortly after my blood counts were confirmed as fine, the infusion prep began.
Once done, my port was flushed and the cannula removed. My nurse reminded me to ensure I start the Filstagrim injections from Friday 26th February. Thanked the team and exited the lounge.
I rushed out as one of my dear friends Dee was outside the hospital waiting for me with some Ghanian-made ginger drinks to hopefully help with my nausea. One of the brews was homemade containing all-natural ingredients and I was looking forward to trying them all. It was so good to see her even though it was for a very short period of time and while social distancing of course.
Today is Monday 1st March 2021: I had a telephone consultation with the Haematology Team at Guy’s Hospital. The call came through at exactly 9:45 AM and a very chirpy consultant from the Haematology Team introduced himself and confirmed if he was speaking with Kemi?
He asked how I had been feeling since a member of their team last saw me? I narrated all I had been going through. From the haematology perspective, I was doing well and all seems to be going as planned since the bone marrow biopsy in early December 2020.
He would speak with my Onco consultant into looking at injecting two Filstagrim injections instead of three but as long as reducing the amount would not interfere with my blood counts to receive Paclitaxel chemotherapy. The thought of that brought a smile to my face. There were a few tips on managing some of my symptoms better and that we would talk again in two months’ time. I thanked him and he hung up.
Today is Wednesday 3rd March: I received my ninth Paclitaxel chemotherapy today at Guy’s Chemo Lounge this morning. As always the process started with a blood test via my port then awaited confirmation that my blood counts are fine for the infusion.
Already comfortable on my chair by the window as always, I was informed by my chemo nurse that all was good and Paclitaxel will be administered.
Starting with an anti-sickness tab and some antihistamine, my readjusted steroids amount, a saline flush followed by Paclitaxel for an hour then another thirty minutes of saline flush.
My port was flushed and the cannula removed. My nurse reminded me to ensure I start the Filstagrim injections from Friday 5th to Sunday 7th March. I thanked the team and left the lounge.
Today is Monday 8th March: My review appointment with Oncology consultant Dr. Hartmut Kristeleit was this morning at Guy’s Hospital.
The electronic board directed me to report to room 24, so I headed there, knocked, and was asked to come. I haven’t seen him in a while so once all the pleasantries were over, he asked if I had a breakout on my forehead? I took off my face covering to show him the extent of the changes to the skin on my face and he was quite shocked. The skin had darkened considerably, I had white-headed sports literally all over the entire face which turned into black sports afterward. The skin around my chin and jawline had thickened and darkened, literally looking burnt. The process had also begun with my hands and feet too.
We went through all that my body had been going through with the side effects since I saw him last about two months ago. He said there was clear evidence that the amount of Paclitaxel chemotherapy being given to me needed to be reduced as my body wasn’t dealing with it too well. He also said the Filstigram injections could be reduced from three to two injections.
The final thing was to examine the lymph node on my collar bone. while checking it, he asked me to confirm the location of the lymph node so I did. I told him I felt it had shrunk and Dr. Kristeleit said “Kemi, it’s more than shrunk, I can feel where it was but I cannot feel the node itself anymore.”
He told me to sit back down while he took off his pair of gloves. He sat down, looked at me then said “Kemi, how would you like to stop chemotherapy?. You have endured so much from this poison and I think it’s time to stop it now. You can carry on with the anti-bodies infusion.” I literally jumped up and thanked him for putting an end to my suffering. I had to control myself because I almost started crying. All that was on my mind was how I was going to cope with the three remaining infusions of Paclitaxel.
Dr Kristeleit confirmed he would send a message to the ENT consultant who would be removing whatever was remaining of the lymph node that it was time to operate. Also that he would request an MRI scan. I thanked him again and with a lighter heart, I left him to get my routine port blood done. I was administered nine Paclitaxel chemotherapy out of the twelve scheduled.
Today is Wednesday 10th March: I arrived at the chemo lounge at Guy’s hospital with a spring in my steps this morning with the knowledge that I would be having the anti-bodies only without Paclitaxel chemotherapy…
My chemo nurse called my name, invited me into the lounge, and asked me to choose a chair for my infusion. While accessing my port she confirmed Paclitaxel chemo had been stopped so I brought her up to date with my meeting on Monday with Dr. Kristeleit. She was very happy to hear about the lymph node shrinkage.
A Call From ENT: A call came through while in the chemo lounge from the ENT department at Guy’s informing me Mr. Alex Rovira would like to see me on Friday 12th March at 1 PM. I accepted the date and time offered. This was followed by a confirmation text.
My port was now ready and my chemo nurse went to request for the first infusion of the seventh session of the antibodies. A flush first, thirty minutes of Pertuzumab, saline then an hour of Trastuzumab, more saline. A long session but not as long as it would have been. I thanked all the nurses and left the lounge with that spring still in my steps.
Today is Wednesday 17th March: I was at Guy’s ENT (Ear, Nose & Throat) Department to see Mr. Alex Rovira, my consultant, and surgeon to remove whatever was left of the node and residue.
He welcomed me chirpily as always and led the way to his office. He asked how I had been and informed me that my Onco consultant Dr. Kristeleit had called and given him the full details of all that had been happening with me. He examined the node and again asked me to confirm its location as he wasn’t able to feel the lymph node either.
He then explained how the operation would be performed and he mentioned that if he found other lymph nodes next to or around the node in question while operating, those would also be removed. I would be spending one night in the hospital as a drain would be inserted at the operation area. He gave me possible dates of when the operation could happen but said he would call me once the MRI scan had been done. He said all would be very soon. I thanked him and left the ENT department.
Today is Monday 22nd March: I received a call from the ENT team informing me of the date for my surgery. Because of COVID-19, my surgery pre-assessment would be online and I needed to complete some online forms and a home COVID-19 test kit would be biked to me with instructions to be handed back to the courier the same day. I thanked Maxine from the ENT admin team and hung up.
Today is Wednesday 31st March: I arrived at London Bridge en route to Guy’s Cancer Lounge super early today because this coming weekend is Easter long weekend and I wanted to treat the nurses that have been taking such great care of me to some Easter cupcakes and Easter eggs.
I arrived at the lounge still in good time with a huge bag of goodies then waited to be called in for my eight antibodies without Paclitaxel chemotherapy.
My chemo nurse called me in and I was asked to choose my chair for treatment. I chose a seat next to the windows, as usual, settled in then handed over the bag with treats to senior nurse Jing whom I know quite well to circulate with thanks.
My port was accessed and prepped for the infusion. A flush first, thirty minutes of Pertuzumab and saline then an hour of Trastuzumab and more saline. My port was flushed then sealed and I was free to leave. Thanked everyone as usual then left the lounge.
Today is Thursday 15th April 2021: Second Vaccination Day!! As the entire world is currently living with COVID-19 and its variations. I’m considered vulnerable because I’m still undergoing treatment and surgery for cancer.
The GP Practise booked me in for the second vaccination jab in the same center as the first time. Again after a rather long wait, it was finally my turn.
This time my vaccination would be administered by a female doctor. She walked me through the vaccination process and how my arm and I may feel in the next few days. Gave me the jab which was again painless, requested my first vaccination card which had my details and what vaccination I was first given, and stock more details of the second jab then handed the card back to me and said I could leave.
Today is Monday 26th April: I arrived at Guy’s Medical Oncology Breast Clinic this morning to get the feedback on the nodes sent to the lab after my ENT neck surgery with Mr. Rovira on the 8th of April.
I was called in by Dr. Kristeleit, already in the office was a breast care nurse whom I have gotten to know quite well. Dr. Kristeleit explained that there were three nodes taken out from my collar bone and the node in question, although had shrunk, still had seven millimetres of HER-2 receptive positive carcinoma inside it and the other two nodes were cancer-free. Normally after chemotherapy, the area would undergo radiotherapy but as the area had already been treated during my first diagnosis, it cannot undergo a second treatment of radiotherapy.
Dr. Kristeleit further explained that as there is no known cancer anywhere else in my body that has been detected, I am now medically declared as in remission. However, I have fallen into a grey area. To ensure that this cancer doesn’t develop anywhere else in my body in the future there were certain steps that needed to be taken.
- 1. My Most Recent Scare
- 2. Chemo Prep The Second Time
- 3. Chemotherapy The Second Time Begins…
- 4. Chemo Side Effect The Second Time
- 5. What I’m Currently Eating
- 6. Port-a-Cath My Saving Grace
- 7. My Lockdown Support Team
- 8. ENT Surgery & Prep
- 9. Chemotherapy The Third Time Begins…
- 10. Chemo Side-Effects & Changes, The Third Time.
- 11. Journey Towards A New Recovery
