"However Kémì, you have fallen into a grey area."
9. Chemotherapy The Third Time Begins…
- 1. My Most Recent Scare
- 2. Chemo Prep The Second Time
- 3. Chemotherapy The Second Time Begins…
- 4. Chemo Side Effect The Second Time
- 5. What I’m Currently Eating
- 6. Port-a-Cath My Saving Grace
- 7. My Lockdown Support Team
- 8. ENT Surgery & Prep
- 9. Chemotherapy The Third Time Begins…
- 10. Chemo Side-Effects & Changes, The Third Time.
- 11. Journey Towards A New Recovery
Dr Kristeleit explained that as there is no known cancer anywhere else in my body detected, I am now medically declared as in remission. However, I have fallen into a grey area. To ensure that this cancer doesn’t develop anywhere else in my body in the future there were certain steps that needed to be taken…
Dr Kristeleit further explained, “the grey area is how we treat you moving on to ensure that there isn’t a reoccurrence in the future.”
“We cannot give you radiotherapy in the same area twice and we cannot be 100% certain that all the residue was removed when the node in question was taken out.”
“So my plan for you is to undergo a preventative treatment process. This is a short term treatment then you can go and live the rest of your life.” I jumped in and asked what would happen if I didn’t take this recommendation going forward. Dr Kresteleit responded, “then you will be on the antibodies indefinitely.”
He then carried on “this will involve having a different set of chemotherapy and antibodies. Because you are still pre-menopausal and your body is still producing oestrogen we need to put your ovaries to sleep permanently to stop the production of oestrogen.”
“The HER-2 receptive positive carcinoma you had is fed by oestrogen and by stopping your body producing oestrogen will mean there will be nothing to aid it to form again. We will induce early menopause.”
The only thing that came out of my mouth was “WHAT?” Nurse Anna moved closer to me as I looked back at her blankly, and said she would go print some information to take home and read.
I looked back at Dr Kristeleit and he went through the plan. “I’d like to put you on chemotherapy and antibodies drug called Trastuzumab Emtansine known as Kadcyla, you will have twelve infusions in total, one infusion every three weeks. This combination will be better tolerated than the last combination with fewer side effects and you will not lose your hair.”
“The injection to put your ovaries to sleep is called Goserelin also known as Zoladex. We are yet to decide when best to start this for now but when you do it will be given once every four weeks.”
“You will also have an infusion of a drug called Zoledronic Acid, and a tablet you can take at home called Letrozole also known as Femara.”
“It’s an expensive treatment and the only thing I haven’t done is put it through to the Board. As soon as that has been presented and approved I’ll give you a call and if it’s not approved there is another avenue I’ll take to get you started on it as soon as possible so there may be a very slight delay if at all any.”
Dr Kristeleit then asked if I had any questions while he handed me the consent forms to sign. I collected the forms, sign and dated them without saying a word because my head just felt like a bomb had gone off in it and I just couldn’t think.
Specialist Onco Nurse Anna had returned holding the printed information by this point and as she handed the information to me then suggested writing all my questions down and relaying them to Dr Kristeleit when he called me if I had no questions for now. I looked at her, nodded and said “ok.”
She then stood up and guided me towards the door. I turned around to look at Dr Kristeleit and he was busy punching away at his computer keyboard. I got his attention again when I said thank you and goodbye. As we walked out he said, “no blood, today but her weight is needed.”
Specialist Onco Nurse Anna and I walked towards the stats room and she handed me over to them and said goodbye. Blankly I acted as instructed by the nurse, put my bag and coat on the chair, stepped on the scale, stepped off the scale, grabbed my things and headed to a corner to put my coat back on before heading out of the cancer building.
I saw Dr Kristeleit on Monday 26th April where he informed me of the new and best way forward in preventing this cancer from ever returning. Since then my head had been in an uncertain fog. I woke up on Thursday morning feeling slightly more myself and with a decision to talk my options through with a doctor at the JP I attended.
Dr Dunstead called me back and I went through all I had been told as accurately as I could remember it. Firstly being thrown into early menopause, having a third (3) set of chemotherapy, antibodies and everything else in between. Together we analysed all aspects of it all and I came to the realisation that this IS the best way forward, an option Dr Dunstead would take herself if the roles were reversed. I thanked her for taking the time and she hung up.
I then called a very close friend of mine aka Mr John who works for the NHS with knowledge of cancer treatment and had another discussion about this new treatment. As soon as I was done with telling him everything he said the treatment was a must and best not to take a gamble with my life.
Feeling a little better and slightly more reassured, I grabbed my bag and took out all the reading materials Specialist Onco Nurse Anna printed out for me a few days ago and read through very attentively page after page. I reread all the information a few more times during the day then made notes.
Today is Wednesday 5th May 2021: Today is the next scheduled appointment for my next set of antibodies in my cancer treatment record book and it’s a 3 PM appointment. As Dr Kristeleit hadn’t called I wasn’t too sure as to what treatment I would be having.
I arrived at the Cancer Lounge early, my treatment nurse called me in and informed me I would be having the new preventative treatment. However because the first infusion would take ninety minutes, the blood test results would take two hours and the pharmacist would also take some time to make the infusion, it was advised to do my blood today and come in tomorrow for the infusion. I agreed.
Dr Kristeleit called Wednesday evening, he apologised for not having called and asked how I had been? I told him and also about my uncertainty of another chemotherapy. He informed me that when my case was presented to the Board, their agreement was unanimous that this was the best way forward for me. He assured me the side effects this time around would be very different and definitely not as harsh and confirmed the funding for my treatment had just been released.
I thanked him for all his efforts on my behalf and he humbly said he was only doing his job. I asked a few questions about the other parts of the treatment, he answered all then confirmed I’d be seeing him in three weeks time, a few days before my second infusion. I thanked him and he hung up.
Today is Thursday 6th May: My preventative treatment Trastuzumab Emtansine (Kadcyla) started this afternoon. I arrived at the Cancer Lounge at Guy’s Hospital and signed in. My chemo nurse called me in and confirmed that all was fine with the blood work done yesterday. My port-a-cath was accessed and the prep for the first infusion began.

Started with my stats which were all fine, a flush for about thirty minutes. Just before my treatment was inserted into my port, I was given one anti-sickness tablet. A few more personal details confirmation and the infusion started. I was observed for the next ninety minutes for any side effects and thankfully there were none. Another flush for thirty minutes and it was all over. One down, eleven more to go.
My combo today was Trastuzumab Emtansine (Kadcyla): A combined targeted therapy and chemotherapy treatment. Used to treat HER2 positive breast cancers that have come back. Trastuzumab is a monoclonal antibody that works by targeting specific proteins (receptors) on the surface of cells. Emtansine is a chemotherapy drug that damages cancer cells.
Just before leaving, I asked how the anti-sickness tabs should be taken and my nurse instructed me to only take it if needed.
Today is Monday 10th May: My appointment with Clinical Haematology Dr Richard Dillon at Guy’s Hospital was earlier this morning. He assured me that from their perspective, I was doing fine and I’m healthy. If this current treatment requires their assistance then my Onco consultant will make a call to haematology again and he would like to discharge me from their care. I agreed, thanked him and left.
Today is Monday 24th May: I decided to go into Guy’s Outpatients department early, to get my blood test done in preparation for Wednesday’s number two infusion of Kadcyla and the start of the ovarian suppression injections. I signed in and was booked for the port blood.
Shortly after that, I was called in by one of the cancer nurses that I had become quite familiar with. My port was accessed and while she got me to confirm my details, I discovered that she was also a Nigerian with a very common Nigerian name.
She had an apprentice nurse watching the process and we all had a good laugh about how common the name Kemi is. Once all was done and the port flushed, I was free to leave. I thanked them both and as I walked out, I prayed my blood counts would come back at the right level for chemo on Wednesday.
I also had a telephone appointment with Dr Kristeleit later in the day and he called me early. He asked how I had been feeling after the first infusion of Kadcyla and I simply replied there had been nothing new in terms of side effects to report but had some questions which he answered gladly. He informed me that the ovarian suppression injection had been changed to a newer medication, he spelt out the name and advised me to read up on it and keep my questions for when I next see him in three weeks time.
He also confirmed my blood counts were fine for the next infusion and concluded by reminding me to start taking the tablets he had prescribed as it works in conjunction with the injections. I thanked him for the call and he hung up.
Today is Wednesday 26th May: I arrived at the Chemo Lounge at Guy’s early, and shortly after signing in senior chemo nurse Ching called me in. We exchanged greetings and I was assigned a place to sit right next to the windows.
My nurse for the day came and introduced herself and shortly after that my port-a-cath was accessed and prepped for my second infusion of Kadcyla. The first ovarian suppression injection would be right after the infusion.
This time around the infusion time was only thirty minutes starting with an anti-sickness tab, a flush before and after. I was then taken into one of the rooms to receive the first of the ovarian suppression injections called Leuprorelin.
This made me extremely nervous and sweaty because I had been informed that the needle is quite big. My chemo nurse noticed my nerves and she just said to relax and not to look at the syringe. As instructed, I popped myself on the bed laying on my back, she wiped the area, pinched some skin on the right side of my lower stomach, and inserted the syringe. The medication was administered slowly which took about three minutes. Three very long minutes.
Before walking out of the room and leaving me to compose myself after the injection, my chemo nurse informed me the area of insertion would be uncomfortable for a few days but would get better. That was probably the most painful three minutes for me in a while.
Leuprorelin (Prostap, Lutrate) is a type of hormone therapy known as an LHRH (luteinising hormone-releasing hormone) agonist. It is used in the treatment of prostate and breast cancer.
Prostate Cancer: it lowers the level of testosterone made by the testicles. Prostate cancer depends on testosterone to grow. So leuprorelin can shrink cancer or slow its growth.
In Breast Cancer: It is sometimes used in the treatment of breast cancer. It is for women who have breast cancer that has oestrogen receptors (ER-positive) and who have not yet gone through menopause (like me).
Leuprorelin lowers the level of oestrogen in the body by stopping the ovaries from making oestrogen. This is because high levels of oestrogen can help cancer to grow.
Today is Monday 14th June: There are two things happening with me at Guy’s hospital today. I arrived really early at Guy’s Out Patients for my port blood in preparation for my next Kadcyla infusion on Wednesday. While the blood taken is sent off to the lab, there is a two hours wait before seeing my Onco consultant Dr Kristeleit.
Dr Kristeleit noticed I arrived early and decided to call me in for an early consultation once the blood work had been done. I walked in and he asked how I had been feeling so I went through my list and questions. I was especially concerned about the existing lump on the side of my stomach from the Leuprorelin injection.
He said the lumps do disappear with time but in some very rare cases don’t disappear at all. On examination, he noted the lump was still quite hard but suggested we needed time to fully assess its situation.
Dr Kristeleit mentioned he received an email from my GP informing him they do not offer the Leuprorelin injection which he requested the GP give me four times a year. They only offer the type given once every month. He found this odd and advised I enquire into how this can be rectified especially if a lump is going to be left after each injection. He would also write back informing the GP of my current situation.
Dr Kristeleit checked and informed me the blood counts were not yet back from the lab. He said he didn’t envision any problems this time but said I could wait if I wanted to. I decided not to wait as he hadn’t envisioned any problems so I thanked him for seeing me so early and left the Cancer Centre with over an hour and a half hours saved.
Today is Wednesday 16th June: As always, I arrived at the Cancer Lounge and signed in at reception, my wristband for the day was printed and I sat in the waiting area of Suit A. Shortly after my chemo nurse for the day called my name, checked my details and invited me into the lounge for a place to sit.
My port-a-cath was accessed and I was given an anti-sickness tablet while the first saline was inserted onto the cannula which was already inserted into my port. fifteen minutes later my lovely Kadcyla infusion was brought out, my personal details were rechecked and it was inserted for the next thirty minutes.
As always I brought the iPad so I turned it on, made myself comfortable and started responding to some emails. I only looked up when the drip timer started beeping, indicating that the fluid had finished. My chemo nurse came to the rescue and informed me there would now be another fifteen minutes of the saline to complete my session for the day.
Again the drip timer indicated the saline was now completed. The nurse came by and informed me I was done for the day. The cannula was removed and my port-a-cath was flushed. I was handed my treatment book with an update of my next appointments then was free to leave.
I packed my bags, thanked everyone and headed out into the beautiful June Mediterranean summer the UK was currently having with temperatures in the thirties.
As soon as I got back into my apartment, I called the GP to request a call back with the very kind doctor I had spoken with a few weeks back when informed I would be having this preventative treatment. She would be available on Friday so will have to call back early to request a call back with her.
Today is Friday 18th June: At exactly 8 AM I called the GP and requested a call back with Dr Dunseath. My phone rang at 9.54 AM and it was the lovely Dr Dunseath calling back. After some pleasantries, she asked what she could do for me and I informed her of the GP letter to my Onco Consultant.
She explained about the GP Red list and how it worked. I informed her of the lump left behind after the first injection and my Onco Consultant’s concerns if I’m to receive a monthly injection. On realising I had already been given the first Leuprorelin injection, Dr Dunseath suggested leaving things with her and she would get back to me next week. I thanked her for her time and we said goodbye.
Shortly after our first call on the same day Dr Dunseath called back and informed me all had been arranged and approved to continue having the Leuprorelin injections with the GP nurse as per my Onco consultant’s request, the date of the first injection would be confirmed in order for the next injection date to be arranged and so on. I thanked her and we said goodbye again.
Today is Monday 5th July: I arrived at Guy’s Out-Patient early for my port blood test in preparation for chemo on Wednesday. My blood counts need to be at the right level for the next hit. I had been seated only a few minutes when my name appeared on the electronic board directing me to room 6.
The door was open and the room was empty so I stood by the door till the port blood nurse instructed me to go in while she picked up the flush for my port-a-cath. She came back and it was a lovely Nigerian nurse who also had a common name, so the familiarity was nice. We exchanged pleasantries while she prepped for the blood extraction. A few minutes later all was done and my port was flushed. We wished each other well and I was free to go.
My telephone consultation with my Onco consultant Dr Kristeleit was for 12.30 PM, however, the call came in early. I was already home from Guy’s so the timing was perfect.
Dr Kristeleit introduced himself and confirmed whom he was talking with. He asked how I had been feeling so I went through my main concerns which were the numbness to my fingers and toes, the rash on the right side of my chest which seems to also be developing near the right armpit, an area that has previously been through radiotherapy, where the lymph nodes had been removed, an area that cannot fight off any infection.
He asked if the rash was itching or tingling and if I could hang on till our next face to face appointment so he could take a look at it. I said yes however if things got really bad I could reach out to the chemo helpline. He confirmed my blood counts were fine for chemo on Wednesday. I thanked him and we said goodbye.
Today is Wednesday 7th July: My fourth Kadcayla was this morning at Guy’s Chemo Lounge. I had received a call the day before asking if my 10 AM chemo session could be moved to 9 AM? I agreed as I’m an early bird anyway. Back at the chemo lounge once called in, I was asked to choose my chair for treatment and naturally picked one next to the windows.
My port was accessed and prepped for the latest infusion. The routine began with a thirty-minute flush, one anti-sickness tab, an hour of Kadcayla then another thirty-minutes flush. My port-a-cath was flushed then sealed and was free to leave. En route out of the chemo lounge, I thanked everyone as always, and with my chemo appointment book updated for the next set of blood checks, Onco consultation and next Kadkayla.
Today is Monday 26th July: I had two appointments at Guy’s hospital today. The first was port blood in preparation for Wednesday’s treatment followed by an appointment with Dr Kristeleit.
After booking myself in for the port blood procedure, I took a seat in the waiting area in Outpatients and kept an eye on the electronic board. Shortly after I was summoned to room 31. I arrived and was met by a new young nurse. She asked me to come in and make myself comfortable while she prepped to access my port-a-cath. My port was accessed and a few minutes later all was done and my port was flushed. I thanked her and left.
I found a seat back in Outpatients to be called to see an Onco consultant in Dr Kristeleit’s team. A nurse I’m quite familiar with had informed me Dr Kristeleit wasn’t in. Although I was a very early arrival, there would be no preferential treatment today. Dr Kristeleit would usually call me into his office if he sees me sitting in the waiting area and I’m very early.
After a rather long wait, I was summoned into a consultant’s room. He introduced himself and asked how I had been feeling since the last infusion. I went through my main concerns and he advised me on how to best cope. There was an examination on my areas of concern, a stronger antihistamine and a new cream to try on my tingling hands and feet were prescribed. Once done, I thanked him and left outpatients.
Today is Wednesday 28th July: My fifth Kadcayla was a late afternoon appointment at Guy’s Chemo Lounge. I was there super early as always and registered at the chemotherapy reception. An armband was printed for my treatment then the waiting began. My chemo nurse finally called my name and before entry, checked my details. I was asked to choose my chair for treatment and naturally picked one next to the windows.
My port-a-cath was accessed and prepped then the routine began. A thirty-minute flush, one anti-sickness tablet given, an hour of Kadcayla then another thirty-minute flush. My port-a-cath was flushed then sealed and I was free to leave. I thanked everyone as always and with my chemo appointment book updated, I headed into the very stormy weather London is currently having.
Today is Monday 16th August: I arrived early at Guy’s hospital today for the first of my two appointments. The first was port blood in preparation for Wednesday’s treatment. Once done, I went back to the waiting area in Outpatients to await a call to see Dr Kristeleit.
The Outpatients department is always busy but I haven’t seen it as busy as this in a very long time and appointments were running a little behind. I saw Dr Kristeleit a few times walking in and out of his office between patients and I was certain there would be no calling me in earlier today so I sat patiently till I was called.
After a rather longer than usual wait, I was summoned into a consultation room. Dr Hannah introduced herself and apologised for the delay and that she would be seeing me on Dr Kisteleit’s behalf. She asked how I had been feeling since the last infusion. There was an examination on my areas of concern which Dr Hannah assured me there was nothing out of the ordinary there.
I asked a few questions and she promised to put them through to Dr Kristeleit. I thanked her and left the outpatients department.
Today is Wednesday 18th August: My infusion today at the Chemotherapy Lounge was an afternoon affair. I checked in at the chemoreception, my treatment armband was printed then I was directed to take a seat in front of Unit B till my chemo nurse called me into the treatment room. I looked around and yet again it was a very busy day, and Unit B was running a few hours behind with appointments.

After the longest ever wait, I was called into the treatment room by my chemo nurse who introduced herself then assigned me to a treatment sofa by the lounge entrance. I made myself comfortable and the treatment process began. Starting with my stats, an anti-sickness medication followed by the accessing of my port. The first thirty minutes was a flush, followed by my sixth Kadcyla infusion for an hour then another thirty-minute flush. My port was then flushed, sealed and cannular removed.
While my chemo nurse was updating my chemo appointment book, I thanked God I was now halfway through finishing Kadcyla chemotherapy. My appointment book was handed back and I left the lounge thanking all the nurses.
Today is Friday 20th August: I had my second Leuprorelin injection this morning at my local GP with the GP’s nurse. Leuprorelin is a hormonal therapy drug used to treat breast cancer in women and prostate cancer in men.
As I’m still very much premenopausal, my body is still producing high levels of oestrogen. Oestrogen can encourage breast cancer to grow. Leuprorelin stops the ovaries from making oestrogen and lowers the level of oestrogen in the body. You only have leuprorelin if you have not been through menopause. You may have it along with other hormonal therapy drugs, or on its own.
I walked down to the GP practice just before 9 AM and arrived on time. COVID-19 has changed everything so as opposed to being let in via the reception area, I had to walk through from the outside to get to the nurse’s office.
I knocked and a very gentle voice asked me to come in. She sat in front of the computer, checking the details of the injection to administer. She asked me to sit down and I handed her the details of the first injection administered at Guy’s and she said all was the same.
Once my details were confirmed she asked me to lay on the bed while she prepared the mixture. I had already applied the numbing cream at 8 AM and covered it with plaster so hopefully, I will not feel the needle going into the skin.
When she was ready, I pulled up my top and upon seeing the plaster she informed me that during training they had been informed that the numbing cream wasn’t advised as it may affect the injection process but not to worry about it.
She gently pulled some skin from the lower side of my left stomach and inserted the syringe. Twenty seconds later all the fluid had been administered and the syringe was slowly pulled out.
There was no pain and very unlike the first Leuprorelin injection three months ago. She went through how the area may feel in the next few days and offered tips on how to best manage my discomforts. I handed her my cancer treatment book and she updated my Leuprorelin injection records and my next due date in three months. I thanked her and bid her farewell.
Today is Monday 6th September: My appointment at Guy’s Outpatients was an afternoon affair. I signed in at reception then informed the nurses that I also needed to have port blood done before or after seeing Dr Kristeleit.
I found a seat after my height and weight had been taken. Looking around I could see it was another busy Monday but not as busy as the last time I was there.
Shortly after I sat down, the electronic indicator directed me to a room number. A lovely young nurse responded to my knock on the door and invited me into the room.
She introduced herself as nurse Annabelle then told me to make myself comfortable while she prepped to access my port.
As she was setting up Annabelle asked what I had been doing and we got talking about rebeKemi. I told her my reasons and aims for starting this site. Nurse Annabelle then revealed that breast cancer was a trait amongst the women in her family. I suggested it may be wise to enquire if she was a high risk as one can now do. Her reply was incredible.
Nurse Annabelle revealed she is unable to make that genetic test request because her mum currently isn’t interested in knowing if she is at a high risk of developing breast cancer and this meant that Annabelle cannot make the request for a check for herself.
Silently I knew nurse Annabelle and I needed to talk more on this issue. I knew I needed to have her on the podcast in rebeKemi, as this was an issue that needed more probing. There must be so many families out there in this same situation.
My port was about to be accessed when one of the breast care nurses knocked on the door and informed me the consultant was ready to see me. With Annabelle’s consent, I picked up my bag and followed the breast care nurse into one of the consultation rooms.
I walked into the room and was met by a new Onco consultant. She introduced herself as Dr Ann Riggs and informed me she would be consulting with me on behalf of Dr Kristeleit.
Dr Riggs asked how I had been since my last chemo infusion?. I gave her an update. She asked specific questions about my appetite and if I had any unusual bruising in the body.
She examined my breasts and concluded all was well. I informed her about my yearly mammogram that was still pending for this year. She assured me a request would be sent to the department for an appointment.
The afternoon team was waiting to start their appointments so Dr Riggs and I had to round up our session. I thanked her and left the consulting room.
I ran back to nurse Annabelle to access my port for blood in preparation for my seventh hit of Kadcyla on Wednesday. I let her concentrate while accessing my port so I didn’t instigate the continued talk about what she had revealed to me, however, once she was finished said she would like to know once rebeKemi went live so I asked for her email address.
Job done. I will ask for her permission to chat on the rebeKemi filmed podcast. With a thankful heart, I promised to stay in touch via email.
Today is Wednesday 8th September: My appointment at Guy’s Chemo Lounge was in the afternoon again. The weather in London town was beautiful and Mediterranean like with a cool breeze. As summer was swiftly coming to an end, I decided to dress up a little. I decided on a very light black spaghetti strap bodysuit with a long floral kimono and a pair of black flat sandals.
I checked in with the chemo receptionist, was given an identification armband for my treatment and was informed of which suit to wait in front of. Shortly after my appointment time, the chemo nurse assigned to me called my name and I went.
I was assigned to a treatment sofa and the process began starting with my stats. My port was accessed and flushed. I was given an antihistamine tablet then saline for fifteen-minute. Confirmation of my confidential details was followed by my seventh Kadcyla infusion for an hour then another fifteen minutes of saline. My port was flushed and my treatment record book was updated. Thanked all the nurses as I left the lounge.
Today is Wednesday 22nd September: Today is my pending mammogram at Guy’s Radiology department. I arrived at the Breast Imaging Department early. Signed in at reception then took a seat till I was called in.
A mammogram is an x-ray picture of the breast. Doctors use a mammogram to look for early signs of breast cancer. Regular mammograms are the best tests doctors have to find breast cancer.
From my first diagnosis with DCIS, I have had a breast mammogram once a year. It’s a little late this year but I can totally understand the reasons for that as I’m sure there must be a backlog due to Mr and Mrs COVID and their variant families.
A very smiley technologist called out my name and I jumped up and followed her into the room. She sat me down and confirmed my personal details. She then instructed me to take off every item of clothing from the waist up and walk towards the x-ray machine once I was ready.
I did as instructed. Now in front of the x-ray machine. The technologist placed my breast on a plastic plate. Another plate firmly pressed my breast from above. The plates then flattened the breast, holding it still while the x-ray was being taken. I felt some pressure and expressed concerns for my port.
There was more movement, pulling of the breast while trying to avoid the port from being caught or pulled by the x-ray machine. The steps were repeated to show a side view of the breast. My right breast wasn’t x-rayed because it’s now an implanted breast. I then waited while the technologist checked the four x-rays to ensure the pictures do not need to be re-done.
Once all the images had been certified as good, I was free to get dressed and leave whenever I was ready. I thanked the two ladies who assisted me and left the building.
Today is Monday 27th September: My appointment at Guy’s Outpatients was yet again an afternoon appointment. I signed in and informed reception that I also needed to have port blood done before or after seeing Dr Kristeleit.
Shortly after my appointment time, I was directed into one of the appointment rooms where I was greeted by a female doctor as Dr Kristeleit was away for the day. She asked how I had been feeling since receiving Cadkyla number seven. I went through my list and she concluded I was looking well with nothing life-threatening, so the treatment continued. I thanked her and walked out of the office to await the call from the port blood nurses.
The electronic indicator directed me to a room number so I jumped up and proceeded towards the room. I knocked on the door and a young nurse asked me to come in. She introduced herself and I noted she was a Nigerian but her name, unlike mine, wasn’t very common.
She asked me to take a seat and confirmed my details before starting the prep for the port blood extraction. She asked how I was and after a very short reply, I redirected the question and discovered she had just returned back to work from having been quite ill.
There was silence while she accessed my port. The port was flushed without any problem but the blood was not flowing like I was accustomed to seeing and before I started panicking she said not to worry that this sometimes happened. She took out another flush and inserted it onto the cannula and pushed it through my port then tried the process again and slowly the blood flow strengthened. We both took deep breaths and exhaled then I remembered the port may have moved slightly during my mammogram session a few days back.
A few minutes later and all was done. I thanked my port nurse and bid her stay in great health and spirit. She smiled and wished me the same. I left Guy’s Outpatient and walked into the street for some fresh air.
Today is Wednesday 29th September: My treatment at Guy’s Cancer Lounge is at 15:30 PM. I will be having Kadcyla number eight and the first Zoledronic Acid infusion.
What is Zoledronic Acid?: Zoledronic Acid is a type of drug called bisphosphonate. It is used to treat osteoporosis. Research trials have shown that Zoledronic Acid can prevent breast cancer from returning in women who have been treated successfully for early breast cancer. Research has also shown that using Zoledronic Acid in postmenopausal women (women who have not gone into menopause) significantly reduces the risk of breast cancer recurring in either the bone or elsewhere and also reduces the risk of dying of breast cancer.
I arrived early and signed in at the chemotherapy reception. My treatment armband was printed and reserved for my chemo treatment nurse this time around. I sat in front of Suite B and waited to be called. I was called in before my treatment appointment time and assigned to a sofa.
My chemo nurse rechecked my personal details then stock the printed armband on my left arm then went through my treatment to ensure we were both on the same page. Once all had been confirmed, my stats were observed and my port was accessed and prepped for the two treatments. After ten minutes of saline infusion, my first ever Zoledronic Acid infusion was inserted onto the cannula for fifteen minutes.
My chemo nurse had pre-warned me on what side effects I may get on receiving the first Zoledronic Acid. I also had to confirm that I had seen the dentist and had a full dental check-up before starting this treatment.
The fifteen minutes went very quickly and before I knew it the dispenser was beeping and my nurse for the duration appeared and confirmed it was all done. After another short saline flush, my eight Kadcyla was brought out, my details re-checked, and the infusion started again for another thirty minutes followed by another ten minutes of flush before the cannula was taken out of my port.
My cancer treatment book was updated and I was free to leave. As always, I thanked all the nurses as I headed out of the chemo lounge and Guy’s.
Today is Monday 18th October: I had a morning appointment to see my consultant and get port blood done at Guy’s. I arrived early at the Outpatients Department, signed in and made it known I would also be needing port blood done.
It was early so I could choose where I wanted to sit. I picked a little corner where I could easily see the monitoring screen. Shortly after my appointment time, the indicator directed me to a room number. I knocked and waited to be called in.
I walked in to see Dr Kristeleit sitting down and by his side also seated was a young lady. Dr Kristeleit introduced her as a student nurse and asked if it was ok for her to sit in on our appointment?. As I hadn’t seen him in a few visits we had our exchanges of pleasantries then quickly got back to the matter at hand.
Dr Kristeleit asked how I had been feeling since my last Kadcyla and first Zoladronic Azid infusion almost three weeks ago. I gave him feedback on how ill I had gotten after the infusions. He explained all the symptoms I had were possible and not out of the ordinary. However, the most important thing was that I was feeling much better.
I expressed concerns about my thinning hair and he explained that it wasn’t the chemo that was affecting my hair, but the ovarian suppression injections; this was the process of what could happen when being forced into menopause. He explained this should stop as my body becomes accustomed to the process. At least that is the hope anyway.
I mentioned having twelve cycles of Kadcyla infusions and the relief that I would be done in December. He checked his notes and corrected me that I would be having fourteen cycles of Kadcyla, which would lead me to February 2022. We talked it through and Dr Kristeleit confirmed it was always going to be fourteen cycles. Sadly and with a heavy heart, I said ok.
We talked about my next ovarian suppression injection with my GP nurse and rectified the dates. I thanked him and the young student nurse. Expressed my delight in being seen by him and left the consulting office to wait for my port blood session.
I was approached and directed to a room by one of the nurses. Knocked and walked in to see the Nigerian nurse that also had a very common Nigerian name. We exchanged pleasantries while she prepped for the port blood extraction and once she was ready confirmed my personal details then started the process.
A few minutes later all was done. My port was flushed and sealed. We talked for a while and I discovered she would be travelling to Nigeria in a few weeks to see her ageing dad. I wished her a safe journey there and back then left the Outpatients department and Guy’s hospital.
En route home, I stopped by my GP to rectify the date of my next ovarian suppression injection then walked home.
Today is Wednesday 20th October: My appointment at Guy’s Cancer Lounge is at 15 PM. I will be having Kadcyla number nine of fourteen and not twelve of as I had originally thought. I arrived early as usual and signed in at the chemotherapy reception then took a seat in the waiting area.
Shortly after my appointment time, my chemo nurse for the day called my name and before assigning me to a sofa, confirmed my details with the printed armband then placed it on my left arm. Once seated comfortably, my stats were checked and my port was accessed in preparation for my next infusion.
Kadcyla number nine started with a thirty minutes saline infusion, followed by an hour of Kadcyla and another thirty minutes of saline. Once done, my port was flushed and sealed. My treatment book was updated and I was free to leave. As always, I thanked all the nurses as I walked out of the cancer lounge and out of the building.
Today is Monday 8th November: My appointment at Guy’s Outpatients today is only to see the port blood nurses. I saw Dr Kristeleit on the 18th of October where we both agreed to see each other again just before Kadcyla number eleven towards the end of November.
On arrival at the Outpatient’s reception, I informed the receptionist that I was only in for port blood. She signed me in and told me to take a seat and keep an eye on the notification board. I did as directed and found a seat where I could easily see the notification board.
Shortly after, my name came up with a room number. I headed there and knocked at the door before being asked to enter. As soon as I walked in, a very chirpy nurse Annabelle greeted me very warmly. For those following my journey, nurse Annabelle and I got into a conversation some months back and I discovered there is a history of breast cancer with the women in her family. I had asked her if she would be willing to have a discussion about it with me on rebeKemi and she had said yes.
Nurse Annabelle had a port blood trainee nurse with her so I let her concentrate on that but we discussed very briefly that we were still good to talk on rebeKemi.
We went through the motions of accessing my port with the trainee nurse leading under the watchful eyes of nurse Annabelle. Shortly after the process was completed and I was free to leave. I thanked them both and left the outpatients department.
Today is Wednesday 10th November:

My appointment at Guy’s Chemo Lounge for the tenth Kadcyla was in the afternoon. I arrived at the Cancer Lounge and signed in at their reception, my name wristband was printed and I was directed to a seat in the waiting area of Suite B. Shortly after, my chemo nurse for the day called my name, checked my details then invited me into the lounge.
Starting with my stats then my port-a-cath was accessed and I was given an anti-sickness tablet while the first saline was inserted into my port. fifteen minutes later my tenth Kadcyla infusion was brought out, my personal details were rechecked then inserted for the next thirty minutes.
The thirty minutes passed by quite quickly, another fifteen minutes of saline to complete my session for the day.
The cannula was removed and my port-a-cath was flushed. My treatment book was handed back to me with an update of my next appointments and I was free to leave.
Today is Friday 12th November: My third Leuprorelin Acetate also known as ovarian suppression injection was at my GP with the GP’s nurse this morning. I picked the earliest appointment time so that I didn’t have too much time to ponder over the actual process.
I arrived early and was met by the same GP nurse that gave me the second injection three months ago. She remembered me and asked how I had been doing since she last saw me. After a brief reply, I redirected the question and discovered she would be leaving the practice soon to focus on a different aspect of nursing. She checked my details and did some updates on her system and in my cancer treatment book.
I was asked to get onto the bed while the content to be injected was removed from the packaging and mixed together. I’d decided from the first injection not to look at the syringe because of the size. This advice came from the chemo nurse who administered the first injection at Guy’s. I remembered her saying “if you look at the needle you will start running and never come back because of how big it is.”
The nurse is now ready and without letting me see the syringe, she wiped the right side of my lower abdomen with a sterile wipe, pinched some skin and inserted the needle while repeating “it’s almost over, it’s almost over, it’s almost over.” A few seconds later the syringe was pulled out and she let go of the skin and put a plaster over the area.
While I got dressed, I thanked her for her services and wished her all the best with what she would be embarking on next. I couldn’t take a gift back to her because Friday was her last day. She walked me to the back door and let me out.
I walked back home slowly and tried to have a normal day while still wondering how bad the side effects would be this time around.
Today is Monday 29th November: My appointment at Guy’s Outpatients today was an early morning visit is to see my oncologist Dr Kristeleit and get port blood in preparation for my eleventh Kadcyla infusion. I last saw Dr Kristeleit on the 18th of October where we both agreed to see each other again just before Kadcyla number eleven on the first of December. I signed in and made it known I would also be needing port blood done before or after seeing Dr Kristeleit.
I sat where I could easily see the monitoring screen which happened to be right next to Dr Kristleit’s appointment office. My name appeared and I jumped up. I knocked and waited to be invited in.
I walked in to see Dr Kristeleit sitting down and by his side also seated was a young lady. Dr Kristeleit introduced her as a student nurse and asked if it was ok for her to sit in on our appointment?. I agreed and he asked me to take a seat. Dr Kristeleit asked how I had been feeling since my tenth Kadcyla and third ovarian suppression injection.
I expressed concerns on the ongoing thinning hair to the temple and middle of my head, while everywhere else kept growing healthily; the ongoing numbness to both hands and feet which hasn’t gotten worse nor better – and told him of the occasional bleeding gum. He informed me the bleeding is a side effect of Kadcyla. My platelet level was low and showing me his screen, said it wasn’t at a level of concern that an eye would be kept on it.
I enquired on when my next Zoledronic Acid infusion would be. I wanted to get the next infusion before my port was removed once chemo was over in February 2022. He again obliged me by saying “yes, it was possible.”
I informed him of the aching right arm, right side of the neck and right upper back. After a few questions on that from him, he asked me to disrobe for an examination. He inspected my neck while talking with the student nurse and indicating where I’d had surgery a few months back, he checked underneath both armpits then asked me to get dressed while he took off his pair of gloves and washed his hands.
He concluded all was well and offered some relief solutions in the form of more medication but I thankfully declined. He also suggested acupuncture to help with my numb hands and feet. This I would give some thought and revert back to him.
Our next appointment would now be in January 2022 before my thirteenth Kadcyla infusion. I requested an early appointment time which he graciously granted. With Christmas and New Year pleasantries over I thanked him, said bye to the young nurse and left the office.
I walked straight towards the port blood nurse’s room, knocked and waited to be invited in. I walked in and who other than nurse Annabelle. She smiled as she asked me to make myself comfortable. As I sat down I noticed although she was in good spirits, she also looked quite tired so I asked how she had been doing.
Nurse Annabelle had been a little ill and although she has recovered still feels quite tired. She’ll be taking a few days off soon to completely rest and she was looking forward to it. Her tray was already prepped as she had been waiting for me. My port access protocol was started in silence.
A few minutes later all was done and my port was sealed. We started talking again and she assured me she was still interested in talking with me on rebeKemi. I asked how her mum has been doing and discovered more revelations to be continued in our upcoming interview. I thanked and wished her strength till her time off happens in a few days time.
Today is Wednesday 1st December 2021: My appointment at Guy’s is again in the afternoon. I arrived early and signed in at the chemoreception then sat in front of Suite B. Shortly after my appointment time, my chemo nurse called my name, checked my details by the door then invited me into the treatment lounge.
As I sat down, my nurse informed me I would be having two infusions, the eleventh Kadcyla and my second infusion of the drug Zoledronic Acid. Dr Kristeleit had put the instructions through!! I’m glad but I’m not looking forward to the side effects as I suffered quite badly with the first infusion.
As soon as I was sitting comfortably, the process began. My port was accessed and flushed, I took an anti-sickness tablet, my details were reconfirmed, the 2nd Zoledronic Acid infusion was inserted for fifteen minutes.
Once done, a fifteen minutes saline, my details rechecked and Kadcyla number eleven was inserted into my port for a thirty minutes infusion followed by another fifteen minutes of saline. My port was sealed and the cannula was removed from it. My appointment book was updated and I was free to leave and as always, thanked everyone as I headed out of the cancer lounge.
Today is Monday 20th December: My appointment at Guy’s today is only for port blood. I will see Dr Kristeleit again in January 2022 just before my thirteenth Kadcyla infusion. Hopefully, if he isn’t too busy today, he may see me quickly so I can give him a little Christmas gift.
As there wasn’t an assigned time, I decided to arrive really early while it was quiet and did my gift rounds while waiting to be called by the port blood nurses.
Finally, my name showed up on the monitor and directed me to a room number. I headed there, knocked then waited to be asked in. I walked in and the lovely nurse Annabelle welcomed me in and introduced me to her port blood nurse in training.
I sat in silence as nurse Annabelle and the trainee port blood nurse worked. The prep first, then the accessing of the port, a flush, blood extraction then a seal before the cannula is removed from the port. Once all was done, I was free to leave so I wished them both compliments for Christmas and the New Year.
Today is Wednesday 22nd December: I had two appointments at Guy’s Hospital today. The first was an appointment at the Cardio-oncology Echo Surveillance Clinic.
Cardio-onco Ech Surveillance aims to prevent, detect, monitor, and treat cardiac complications in patients with cancer or receiving cancer therapy. Transthoracic echocardiography is the key diagnostic tool for screening, surveillance and detection.
A technician (sonographer) spreads gel on a device (transducer). The sonographer presses the transducer firmly against your skin, aiming an ultrasound beam through your chest to your heart. The transducer records the sound wave echoes from your heart. A computer converts the echoes into moving images on a monitor.
My second appointment was at the Cancer Lounge for Kadcyla number twelve. I signed in at the chemoreception then waited to be called in by my chemo nurse for the day. My name was called, my printed wristband checked, then I was invited into the lounge. I made myself comfortable, then handed over the bag of Christmas treats for all the chemo nurses.
The routine was the same as always, starting with my stats, followed by the accessing of my port and prepping it for the infusion. Then there was the fifteen-minute flush, an anti-sickness tablet followed by Kadcyla number twelve for thirty minutes. Then finally, another fifteen-minute flush. My port was flushed, sealed and cannula removed. I said a thank you to the nurses, wishing them a Merry Christmas and all the best for the New Year as I left the Cancer Lounge.
Today is Wednesday 5th January 2022:

My appointment early this morning was at the dentist. My current treatment requires that I get regular checks by dentists and hygienists. I see the hygienist for a polish twice a year anyway, the only difference now is that the process is being recorded. An hour later all was done with my mouth and teeth feeling refreshed.
Today is Monday 10th January: My first appointment at Guy’s this year is to see Dr Kristeleit and to also get port blood done in preparation for my thirteenth Kadcyla infusion. It was an early appointment, but I could see patients arriving as the waiting area filled up.
Dr Kristeleit called me into his office as he walked back in, and after exchanging New Year’s pleasantries, he asked how I had been doing so I went through my list of events after having the second infusion of Zoledronic Acid last year. As he had earlier assured me, the side effects were not going to be as bad as the first time around, but I still went through my list.
He was encouraging, commending and sympathetic with all I had gone through. He said it was almost over and that Kadcyla would remain in my system for about six months once treatment was over and I should start noticing some definitive improvements by then. Unlike other chemotherapies, Kadcyla’s side effects wore off more slowly.
Just before I left his office, I decided to inform Dr Kristeleit about my little project rebeKémì and he seemed genuinely interested. I informed him I would like his involvement at some stage. While he didn’t make any promises, he said to reach out when I was ready. We talked a little about cancer treatment in Nigeria and his experiences with patients coming into the UK for private medical care. He offered some direction on focal points worth considering and wished me luck. I thanked him for all he had done while treating me this second time around and left his office.
Today is Wednesday 12th January 2022: My appointment at Guy’s this morning was the first for this year at the Cancer Lounge. I arrived early as always and checked in at their reception. Shortly after, my chemo nurse for the day called my name, checked my wristband and invited me into the lounge. I picked a treatment sofa by the window and made myself comfortable. Although the weather was cold, the sun was out and bright which gave a Spring-like feel to the lounge.
The routine was the same as I remembered it – starting with my stats. Once my port was accessed and prepped, the first fifteen minutes of saline was inserted, an anti-sickness tab taken and after a rather long wait because the pharmacy was slightly behind in time, Kadcyla number thirteen was inserted for thirty minutes. There was another fifteen minutes of saline and it was all over. My port was flushed and sealed and I was free to leave.
Today is Monday 31st January: I arrived at Guy’s Outpatients for my last Oncology appointment and to also get port blood for the last time too. It was an early appointment so the waiting area was quiet. Shortly after my height and weight were taken I was summoned to consulting room 34, which I noted wasn’t Dr Kristeliet’s.
I knocked at the door and waited to be invited in. I was welcomed by a female oncology Doctor that I had met on a previous occasion. She introduced herself and asked how I had been doing and feeling. I went through my list and she assured me things should start getting back to some form of normality six weeks after Kadcyla.
Although I was really scared of the answer to this particular question, I needed to hear the specialist’s views so I asked if I was done dealing with cancer?.
She talked me through my journey, starting from five years ago, and pointed out how rare it was to get a subsequent diagnosis that could be so easily treated and removed. With the other preventative treatments to continue for the next couple of years, she was very optimistic it would not happen again.
I then asked her to define her optimism in percentage form and she said 95% optimistic. She said to continue to take great care of myself and my body, and should I ever need to alert the oncology team of anything, to use the contacts I had been given.
She said it was always a pleasure to see patients at the end of their treatment to be able to wish them well. I would be put on the waiting list to have my Port-a-Cath removed, so I should expect an invitation within the next few weeks. I sent my regards and thanks to Dr Kristeliet and she promised to let him know. I thanked her again and left the consulting room.
I walked back to the waiting area and waited to be called in by one of the port blood nurses. Shortly after, my name showed up on the monitor and directed me to a room number. I headed over, knocked, then waited to be asked in, where I was greeted by a nurse I was seeing for the first time.
She invited me in and introduced herself while she prepared for the blood extraction from my port. A flush, blood extraction, then a seal before the cannula was removed from the port. Once all was done I was free to leave, so I wished her well and left the building.
Today is Wednesday 2nd of February. My appointment at Guy’s Chemotherapy Lounge this morning is to receive Kadcyla number fourteen. This will be my final infusion. With it will be my third Zoledronic Acid – my first for this year. As I get two infusions a year, I’ll be back for another dose in six months time.
I signed in at the chemo reception, then waited to be called in by my chemo nurse for the day. My name was called, my printed wristband checked, then I was invited into the lounge.
The routine was the same as always, starting with my stats, followed by the accessing of my port and prepping it for the infusion.
I had the Zoledronic acid infusion first. A fifteen-minute flush, Zoledronic acid infusion for thirty minutes then another fifteen-minute flush.
It took a while for the pharmacy to prepare the last Kadcyla, and by the time it arrived, I had already taken an anti-sickness tablet, so it was connected to my port. An hour later and all was done. Another fifteen-minute flush, my port was sealed and cannula removed.
Sadly today’s treatment was administered by a nurse I didn’t know and none of the regular nurses were around to thank and say goodbye to, so I just thanked the chemo nurses of the day as I walked out of the Cancer Lounge.
It was such a relief to know that I was now done with the monthly infusions. Thank God!
Today is Monday 7th February. I had my fourth injection of Leuprorelin Acetate, i.e. the ovarian suppression injection with the GP nurse this morning. On my previous injection day in early November, the nurse had mentioned it was her last day, so I was looking forward to meeting the new nurse.
I arrived at the GP early and waited to be called in. A young lady called my name and escorted me into her station. She introduced herself and I asked if she was the new nurse – she said it was yet to be decided. She confirmed my details while looking at her screen then asked me to lay down while she prepared the injection.
I never look at the syringe, so with closed eyes, I pulled up my top revealing the lower part of my belly and felt as she got closer. We both confirmed which side to inject and I heard her say “you poor thing, you are so tiny”. She wiped the left side then pinched some skin. A few seconds later, it was all over and a plaster was placed over the area.
We confirmed the date of my next injection, which would be in twelve weeks. I made note of it, wished her luck on her could-be new post and bid her goodbye.
Today is Monday 14th March. I received a call from the Radiology & Intervention department regarding getting my port-a-cath removed. A few dates were suggested and we finally agreed to a date in April. There are a few steps to the process and all was arranged and confirmed.
Today is Monday 11th April. I had an appointment at Guy’s Hospital this morning to have a face to face with one of the pre-assessment Nurses at the Interventional Radiology Department.
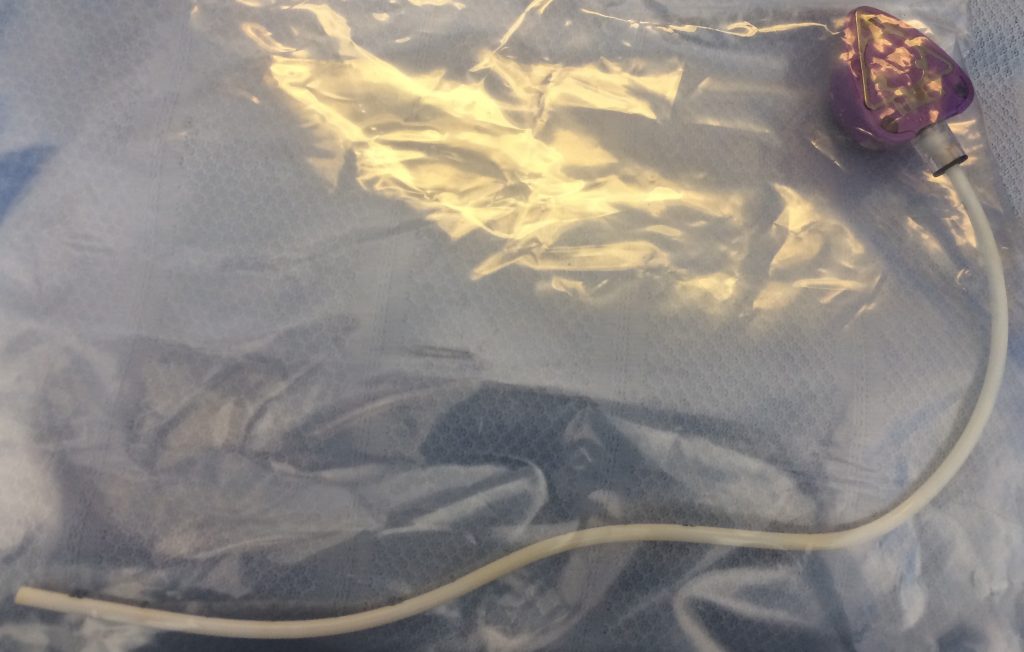
For those that have been following my journey, you’ll know that I had a port fitted in order to receive chemotherapy without having to worry about being pricked several times with a needle, as my veins are really small and sometimes disappear once the needle touches them.
I’m happy to announce the time has now come to have my port taken out as the monthly infusions of chemotherapy are now finished.
On arrival, the receptionist handed me some forms to fill in while I waited to be called in by the nurse. I sat down, looked at the forms and started answering the multiple choice questions.
I was on the last page when I heard my name and jumped up. The pre-assessment nurse introduced herself and asked me to follow her. We walked into her office and she took the forms from me then started asking questions while she went through it.
Once the questions were all answered, she went through the port removal process and informed me I would be awake for the procedure. She conducted the necessary swabs then informed me she would also be taking some blood. I wanted to get up and run for the doors, but I managed to stay calm and seated.
She tried to find a vein twice but failed to get any blood flow before going to look for another nurse who also tried twice without any luck. She apologised and informed me I would need to visit the central blood withdrawal department located in the next building. She handed me the blood sticky labels and I left the pre-assessment department.
I walked into Guy’s Cancer building and into the blood department. There were quite a few people, so I waited until a nurse became available to talk with. I gave her my forms and sticky labels, then she walked me into a cubicle and introduced me to a lovely young woman who would be performing the process.
After confirming my details, she asked where would be best to try again. I showed her and she tried once and got a good flow of blood. While this was happening, I noticed how her face covering had been held up at the back of her hijab instead of inside it.
I told her it was a very clever idea to have the piece of fabric with two buttons, one at each end keeping her face covering secure and more so she wouldn’t need to tamper with her hijab while removing the face covering, or putting it back on. She smiled and said she had made it herself. I mentioned there may be some money in that and we both laughed.
Once the young phlebotomist was done, she covered the area with a plaster and I was free to leave. I thanked and wished her a great day in Arabic. Surprised and in laughter, she responded back as I carried my bag and walked off.
Thankful this part was finally over. I exhaled and headed towards Borough Market ahead of the lunch hour to walk around before heading home.
Today is Wednesday 13th April. I had a routine appointment at the Cardiothoracic Centre this morning at Guy’s hospital to have an echocardiogram. Kadcyla chemotherapy can sometimes affect the heart, so this is just to ensure my heart is still doing very well.
I arrived early and signed in at reception. I was first called in to get my height, weight and blood pressure done. All was normal there so returned to the waiting area to be called in for the echocardiogram.
Echocardiography uses ultrasound waves to create a picture of the heart, called an echocardiogram (echo). It is a noninvasive medical procedure that produces no radiation and does not typically cause side effects.
During an echocardiogram, a doctor can see:
- the size and thickness of the chambers
- how the valves of the heart are functioning
- the direction of blood flow through the heart
- any blood clots in the heart
- areas of damaged or weak cardiac muscle tissue
- problems affecting the pericardium, which is the fluid filled sac around the heart
The sonographer called my name just as I sat down and I jumped up to follow her. As she introduced herself, I realised she was the same consultant who conducted the same test six months ago. I told her so and she said she remembered me too. She asked me to take off everything on my upper half and put on the hospital robe, then lay down.
The process was very simple and straightforward, just as I’d remembered it. A gel used especially for scanning was used to help the sound waves reach the heart. It felt cold and sticky.
The sonographer moved the probe over different areas of my chest around my heart. The probe gives off pulses of high frequency sound waves, which pass through the skin to the heart. The ultrasound waves ‘echo’ against the structures of the heart and the probe picks up these reflections and shows them as images on a screen.
Different parts of the heart are seen as the probe is moved around on my chest. Every now and then, I was asked to breathe in or out while holding my breath. Fifteen minutes later all was done and I was given some tissue to wipe off the clear gel. She told me all looked good and all the images would be sent to my consultant. She also informed me I would need to see her again in six months time for a final echo.
I thanked and wished her well, then got dressed and left the cardiothoracic department.
Today is Thursday 14th April. Port removal day! I was requested to be at St. Thomas’ Hospital by 8AM, so I was up by 6AM. I walked out of Westminster underground station at 7.35AM – the sun was already out and very strong. The view of the Houses of Parliament and the London Eye across Westminster Bridge was spectacular.
At the entrance of St. Thomas’, I took out my letter with directions and looked for the Interventional Radiology Department, located on the 1st Floor of the Lambeth Wing.I arrived to an almost empty ward, with just one gentleman there that had arrived before me. We acknowledged each other with a nod and I stood behind him. A few minutes later a senior nurse came through and took him. He then came back for me a few minutes later. He walked me to a cubicle with a bed and a chair and asked me to sit and wait.
A young nurse walked into the cubicle and introduced herself as my nurse for the day. She had the same name as my younger sister, Wunmi. Interestingly enough, I looked at her as she walked away, then again as she walked back to me with some forms, a hospital gown and a pair of socks. She was shaped and looked so much like MY Wunmi that they could easily be twins. They even sound alike with the same mannerisms. It was almost scary. I just stared at her as she instructed me on what to do. I had to tell her so she didn’t think there was something else wrong with me as I just kept staring.
Nurse Wunmi then informed me she would need to insert a cannula into the back of my left arm as she looked at the left hand. I panicked and quickly told her how difficult a task it could end up being, so she advised that the surgeon would probably be best to try just before the port removal starts. I agreed… And I exhaled.
She closed my cubicle and I got changed, then put my belongings in a green plastic bag. She came back and went through the forms with me, filling out the details as I gave her my answers. Once done, I signed and dated the forms. She said to sit tight and my surgeon would be in shortly to go through the port removal procedure. I nodded and she walked out again.
About ten minutes later, friendly doctor walked in and introduced himself alongside his attending doctor. They both went through the process and confirmed I was aware of what was to be done. I signed two more forms and they both went into the next cubicle. About another ten minutes later, nurse Wunmi came back and told me I would be going into the theatre very shortly.
Another nurse came into my cubicle and we walked into the theatre together. There were three nurses, my port removal surgeon and his senior doctor. I was asked to lay on the operating table while the nurses positioned and covered me up. I was told a scan needed to be taken first to check the positioning of the port valve, so everyone left the theatre for this, then they all re-entered and carried on.
There was a lot of movement and talking, tools were being removed from drawers, monitoring stickers were placed on my chest, back and sides and when all was ready, everyone came near and introduced themselves. Sadly, not one name stuck as I was busy praying, while nodding at each one of them.
My left chest was sterilised and a huge blue sheet was placed on it. There was an open space where the port was to be removed. My surgeon then informed me there would be a few stings as he made the area numb, but after that I should only feel pushing and pulling.
About twenty minutes into the removal he moved closer and asked how I was doing, then informed me the hardest bit had been accomplished and he only needed to remove the base to the port. I thanked him then started praying again.
I then decided to tell him about what I had discovered about the port when it was first introduced to me in late 2020. He was astonished that I knew so much about the evolution of the oncology port. Its original aim was to help babies with eating difficulties; it’s now evolved in order to be used for different procedures today. He called the nurses and was telling them how much I knew about my port.
I then asked if it was ok for me to take a picture of the port and he said yes, I could take a picture, but I wasn’t allowed to take the port away with me. He again called on the nurses and asked them to ensure I was able to do as requested.
The base of the port was now out and he stitched up the area. I heard the nurses counting the tools used, then everyone walked out while an x-ray was taken to ensure all had gone well. Everyone came back and I was cleaned up and wheeled back to my cubicle in the recovery room.

I was to be observed for an hour. During that one hour observation period, my stats were recorded every fifteen minutes. I was also offered something to eat and drink. Once my observation period was over, nurse Wunmi informed me it was fine to slowly get out of bed, get dressed and make contact with my pickup person. She also took off all the monitoring stickers that had been strategically placed all over my top half.
I stepped out of bed slowly and sat on the chair next to the bed. I took my mobile out of my bag and turned it on. I picked up the little see-through plastic bag that had the port inside it, placed it on the bed and took a few shots moving it around a few times. It reminded me of something out of a horror movie.

I made a quick call to my darling sister from another mother, Jane, then sent my other sisters a text that all had gone well and I was waiting to be picked up.
Once dressed, I walked slowly into the bathroom and back to my cubicle feeling fine, but quite tired. I was asked to move into the waiting area while I waited to be collected, so I slowly packed my belongings, walked there, found a comfortable sofa and sat down.
My adorable sister, Jane walked in and started checking me over to ensure I was well enough to leave. I took her to nurse Wunmi to be discharged and even Jane couldn’t miss the resemblance between the two Wunmis, and also told her so. I was certified to leave, so off we went, leaving St. Thomas’ Hospital into the beautiful sunshine and glorious views over Westminster Bridge.
En route home, Jane persuaded me to stop and have a quick bite at one of our favourite places while we caught up a little. We did, and I’m glad and thankful we took that time. After getting home I had an early night, feeling thankful the day had gone without any hiccups.
Today is Thursday 28th April. My port was removed exactly two weeks ago today, but I’ve yet to receive a call from the nurse to get my stitches removed. I decided to call the specialist breast care team to alert them. The protocol is to call their line, leave my details at their call centre and then one of the specialist breast care nurses would call me back.
Shortly after, that same morning, one of the breast care nurses called back and after listening to my concerns, she advised me to leave things with her and await a call back. I thanked her and she hung up.
Today is Friday 29th April. I received a call from the Interventional Radiology Department at Guy’s. It was the same nurse that had removed my stitches in 2020 when the port was first inserted. She informed me that she had gone through my Port-a-Cath surgical removal notes. There were no stitches this time around as the consultant had used glue; there was no need to come back to the hospital. She advised me to keep changing the dressing as required.
I informed her of my upcoming Race For Life run and pleaded to kindly have some more dressing to have the area well protected while I was training. She very kindly agreed to leave a little pouch for me at the reception in Guy’s with my details, to be collected at my convenience. I thanked her and we hung up. The dressings were picked up the following Monday.
Today is Tuesday 3rd May 2022. I had my fifth Leuprorelin (Prostap3) injection this morning with the GP nurse. The ovarian suppression injection was given by the same nurse from three months ago. She remembered me, and I her. I congratulated her on retaining her new post as the new nurse. She checked my details, confirmed which side of my stomach was to be injected, and the dose.
Again, she mentioned how tiny I was with very little body fat, then suggested instead of laying flat on my back for the injection, to sit up and slouch forward so the belly fat would be more visible. I assumed the position, pulled up my top, then shut my eyes. I felt her move closer, wipe the area, then pull at the skin. There was a prick, and a few seconds later, all was done.
I opened my eyes and watched her put a plaster over the area. She very kindly decided to order some numbing cream for me for the foreseeable injections. I almost jumped up to hug her, but I settled for a very gratifying thank you. We both agreed on the date for the next injection in three months time. I thanked her then exited the GP surgery via the back exit.
Today is Thursday 5th May. Today marks three weeks since my Port-a-Cath was removed at St. Thomas’ Hospital’s Interventional Radiology. After my early morning run, I decided it was time to take the dressing off from the area where the port was removed.


After a quick shower, I smothered my body in my favourite Kieh’s body moisturiser, stood in front of the mirror and very carefully peeled the plaster off. Taking a closer look, it looked very flat and was healing quite nicely. The area remained very tender, so I was tempted to keep it covered up before going to bed and running. For now though, I shall leave it uncovered; another hurdle that I’m nearly over.
- 1. My Most Recent Scare
- 2. Chemo Prep The Second Time
- 3. Chemotherapy The Second Time Begins…
- 4. Chemo Side Effect The Second Time
- 5. What I’m Currently Eating
- 6. Port-a-Cath My Saving Grace
- 7. My Lockdown Support Team
- 8. ENT Surgery & Prep
- 9. Chemotherapy The Third Time Begins…
- 10. Chemo Side-Effects & Changes, The Third Time.
- 11. Journey Towards A New Recovery
